Hypoglycemia and Medical Cannabis Treatment
- What are the Signs, Symptoms, and Types of Hypoglycemia
- Hypoglycemia: Causes and Complications
- Are Cannabinoids a Good Treatment Option for Hypoglycemia
- How Does the Endocannabinoid System (ECS) Play a Role in Treating Hypoglycemia
- What Cannabis Preparations are Suitable for Hypoglycemia?
- Talk to Your Doctor About Hypoglycemia Treatments
35Glucose (blood sugar) is the human body’s main energy source; the whole system is disrupted without the right amount. When levels of glucose fall below the standard range, a condition known as hypoglycemia occurs. One to two per 100 people diagnosed with diabetes annually visit a hospital to treat severe hypoglycemia. It can likely be a significant risk factor for earlier death (20).
To understand whether or not your fasting blood sugar is at a dangerous level, you must first pay attention to the warning signs and glucose levels, if possible. When a fasting blood sugar measures 70 milligrams per deciliter (mg/dL) or drops to 3.9 millimoles per liter (mmol/L), the CDC recommends that you quickly consume 15-20 grams of glucose or carbohydrates and recheck your glucose levels in 15 minutes. This is called the “15-15 rule (3).”
You may need to contact your doctor for hypoglycemia management, use an emergency glucagon pen, or contact emergency services — especially if you lose consciousness, have a glucagon injection, wear a medical ID, or don’t respond to oral glucose. Refer to the CDC guidelines for when to call 911 (3). Since the consequences could be severe, it’s essential to consult a healthcare provider and avoid hypoglycemic events if you know you have diabetes.
Treatment for hypoglycemia usually involves following a particular health and wellness plan to get your health back on track. A doctor will help you follow a proper diet and medication plan to promote a normal blood sugar reading.
They may also refer you to a diabetes education counselor, a helpful guide who can discuss your diagnosis, nutrition, medications, medical devices, and how to manage your diabetes best and prevent hypoglycemia. Severe or repeat hypoglycemia may need a specialist referral to an endocrinologist.
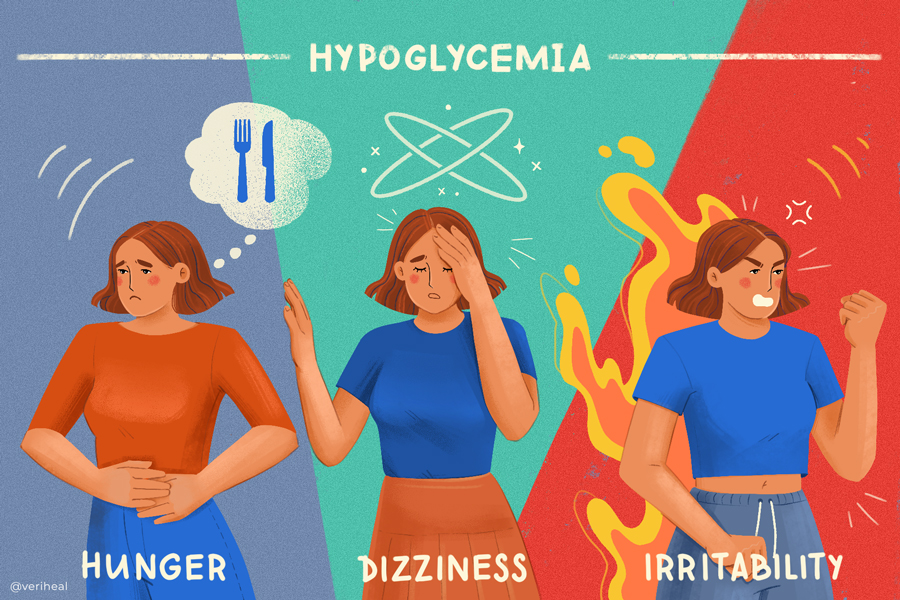
What are the Signs, Symptoms, and Types of Hypoglycemia?
According to data from the CDC, in 2018, approximately 17 million ER visits were reported with diabetes as any listed diagnosis among adults. Of this number, 248,000 visits were for hyperglycemic crises (~10 per 1,000 adults with diabetes).
Data from the same year shows that of the 8.25 million hospitalizations with diabetes as any listed diagnosis among US adults, 60,000 hospitalizations were for hypoglycemia (~2 per 1,000 adults with diabetes) (4).
Although it is uncommon in people who have diabetes, hypoglycemia has also been connected to the use of other drugs and a variety of rare conditions. In any case, hypoglycemia requires immediate medical attention, likely even self-administered if you know what to do.
Although people who have diabetes, particularly if poorly managed or with significant cost or insurance barriers, are more likely to develop hypoglycemia. It is also more likely in those who struggle to maintain a good food regimen, exercise routine, struggle with poverty, unemployment, live in a food desert, lack access to healthcare, or have a contraindication to prescribed meds. However, it is also possible for people without diabetes to experience the symptoms of hypoglycemia.
Doctors will usually diagnose a patient with one of two different types of nondiabetic hypoglycemia, which is then graded into three levels (mild, moderate, and severe). They are as follows:
- Reactive Hypoglycemia – The symptoms of this type of hypoglycemia usually erupt a few hours after eating a meal high in carbs.
- Fasting Hypoglycemia – If a person experiences hypoglycemia after abstaining from food for eight hours or longer, they may be diagnosed with fasting hypoglycemia (6). Severe disease or medicines (e.g., too much insulin, aspirin, etc.) are two common contributing factors: binge drinking, thyroid or endocrine disorders, and less likely tumors.
- Mild Hypoglycemia – Being aware of the symptoms of mild hypoglycemia, such as headache, sweating, and a pale complexion, means that you can treat it without obtaining doctor-approved medication (13). Mild cases can be resolved by making basic lifestyle changes, such as increasing sugar intake to amplify the body’s fuel source.
- Moderate Hypoglycemia: Depending on the severity of your blood sugar reading, a doctor may need to assist you in restoring glucose levels. Mild-to-moderate hypoglycemia (blood glucose < 4.0 mmol/L) is best treated with 15 g of carbohydrates. The treatment should be repeated if symptoms don’t diminish within 15 minutes (14). Patients should keep snacks at home, work, and school to prevent these episodes. At this stage, patients may check their blood sugar regularly and be prescribed glucagon pens in case of emergency to avoid the next stage.
- Severe Hypoglycemia: Patients with severe hypoglycemia risk going into a coma. This type of hypoglycemia is considered a medical emergency. Dangerously low blood sugar levels should not be treated with rapid sugar uptake since this may result in hyperosmolar syndrome and hypokalemia, thus increasing the chances of other health complications arising (11). If you fall into this category, you should ask family or friends for help, use a glucagon pen, call local emergency medical services (911), or visit the nearest emergency room for intravenous glucose. Do not attempt to drive yourself as you could easily pass out and cause a worse situation.
When blood sugar levels start to drop, the following signs and symptoms of hypoglycemia will usually surface:
- Anxiety
- Difficulty concentrating
- Dizziness
- Fatigue
- Heartbeat irregularities
- Headache
- Hunger
- Irritability
- Lightheadedness
- Lip, cheek, or tongue numbness/tingling
- Nausea
- Pale skin
- Shakiness
- Sweating (13)
If hypoglycemia worsens to a dangerously low level, symptoms include:
- Confusion, unusual behavior, or both, such as the inability to complete routine tasks
- Loss of coordination
- Slurred speech
- Blurry vision or tunnel vision
- Nightmares, if asleep
Severe hypoglycemia may result in the following:
- Unresponsiveness and loss of consciousness
- Seizures
Hypoglycemia: Causes and Complications
As mentioned above, diabetes is not always the cause of hypoglycemia, even though it is a common cause. Not eating a well-balanced diet (fasting), taking too many diabetes medications or other prescription medications, or being malnourished increases the risk of low blood sugar levels.
Hypoglycemia may also surface as a complication of pregnancy, binge drinking, weight loss surgeries such as gastric bypass, critical illness, or various other medical conditions, including hormonal imbalance or health complications related to the adrenal glands, heart, kidneys, liver, or pancreas (15).
According to MayoClinic, some of the most common complications of untreated hypoglycemia include unresponsiveness (loss of consciousness), seizures, or even death (13). Regardless of the pathways to the infection, it’s important that you make yourself aware of the dangers of not getting treatment.
As hypoglycemia intensifies, several health complications may surface, including seizures, unconsciousness, and death. This is particularly true in cases where the patient does not seek suitable treatment quickly.
Are Cannabinoids a Good Treatment Option for Hypoglycemia?
Most healthcare providers treating someone with hypoglycemia will prescribe a medication called glucagon – a type of hormone that promotes blood glucose release from liver glycogen stores. This medication may be squirted up the (nasal cavities) or injected with a needle.
Cannabis could also help with managing your blood sugar levels. According to Medical News Today, the leafy plant has been associated with stabilizing blood sugar, enhancing circulation, reducing neuropathic pain, and lowering blood pressure. Plus, the American Alliance for Medical Cannabis (AAMC) notes that cannabis can help to keep blood vessels open, which may effectively reduce blood pressure (1). There is early preclinical research and a small research study to support this (12, 10).
Since hypoglycemia may also cause gastrointestinal problems, the primary non-psychoactive compound in cannabis, cannabidiol (CBD), and its acidic precursor, cannabidiolic acid (CBDA), could prove helpful in suppressing nausea and vomiting within a limited dose range (18). Other cannabinoids with promising regulation of pain, GI propulsion, and nausea and vomiting regulation include THC, THCA, CBCA, and more (21).
Further research indicates that cannabis users have lower levels of fasting insulin. The findings, which were published in the American Journal of Medicine under an article titled “The Impact of Marijuana Use on Glucose, Insulin, and Insulin Resistance among US Adults,” explored the blood sugar-associated effects of cannabis consumption among 4,657 study subjects in the National Health and Nutrition Examination Survey from 2005-2010 (16).
The researchers found that current cannabis consumers had “lower levels of fasting insulin, lower levels of insulin resistance, smaller waist circumference, and higher levels of HDL cholesterol, which is known to reduce the risk of cardiovascular disease.” In this study, however, no effects were found on blood sugar.
Conversely, five different studies found that glycated hemoglobin (HbA1c) was higher in people with type 1 diabetes (T1D) who used the plant in recreational form (17). Excess sugar present in the blood attaches itself to hemoglobin over time, causing an elevated A1c over time. Unfortunately, this review only covered six total observational studies and weakly associated potentially worse outcomes for T1 and T2 diabetes that need to be studied in larger populations.
However, a larger and more recent 2016 study learned that the cannabinoids CBD and THCV significantly lowered blood glucose levels and amplified insulin production in type 2 diabetes patients (9). This is relevant since insulin is an essential hormone that humans cannot survive without — it promotes the body’s blood sugar intake, which is then used for energy. Not only this, but insulin also instructs the liver to conserve blood sugar for later use; insulin is commonly prescribed in diabetes (2).
Understanding the role of cannabinoids in changing blood sugar levels can help us figure out how to treat diabetes better and perhaps prevent complications. Collectively, these findings suggest that some cannabinoids (but not all) may be an effective option for helping hypoglycemia, especially as an appetite stimulator. Knowing which cannabinoids to choose will be helpful someday as research advances.
However, the plant should not be considered an established, approved treatment for diabetes nor a cure. More research is needed into how we can better select cannabinoid targets to modify blood sugar levels and potentially change the course of someone’s diabetes.
How Does the Endocannabinoid System (ECS) Play a Role in Treating Hypoglycemia?
The endogenous cannabinoid system (ECS) controls the regulation of energy homeostasis, as well as the regulation of glucose homeostasis. Research demonstrates that homeostasis plays an essential regulatory role in hormone secretion. The most vital elements of the ECS are CB1 and CB2 endocannabinoid receptors.
Endocannabinoid receptors are essential for controlling energetic balance mechanisms, and when they are not stimulated or overstimulated, the system can become disrupted. These receptors are spread around the central and peripheral nervous system and in various peripheral tissues.
Early but mounting evidence points to the fact that an overactive ECS, particularly CB1 overactivation, may increase diabetes development by influencing energy intake and storage, releasing pro-apoptotic effects in pancreatic beta cells, causing inflammation in pancreatic islets, and hindering glucose and lipid metabolism (7).
The key will lie in understanding the differences between CB1 and CB2. They are still being worked out, but too much CB1 activation in organs like the liver and pancreas is bad and causes more inflammation and cell death (apoptosis). However, learning adverse facts in research is very important because researchers can use that to figure out how to make or find cannabinoids that trigger the opposite. CB2 may help do so.
CB2 activation in preclinical studies improves inflammation associated with obesity and diabetes. So new diabetes and cannabis research will need to look into how they work differently and how we could block CB1 while stimulating CB2 (19). Similar differential actions may be happening in liver disease. This may be why CBD and THCV may be promising candidates since they modify and partially block normal THC action at CB1 while having some weak, partial action at CB2.
Additionally, hypoglycemia associated with diabetes has also been involved in disrupting the aforementioned pathological processes related to the ECS. To prevent the ECS from going out of whack, researchers should broaden their knowledge of these mechanisms and their connection with developing new therapeutic approaches for hypoglycemia.
What Cannabis Preparations Are Suitable for Hypoglycemia?
Smoking marijuana is not the only way for patients with hypoglycemia to use cannabis. In fact, smoking any substance should be avoided to minimize cardiopulmonary side effects.
The diversity in cannabis preparations means that there truly is something for everyone. Pills, capsules, tablets, tinctures, and vapes are recommended for fast-acting relief from the plant’s active compounds. In contrast, edibles and water-soluble cannabinoids offer longer-lasting symptom relief, but these products take longer to experience effects.
Topical formulations like balms, creams, and salves may also offer symptomatic relief from diabetic nerve pain, according to a small 2020 clinical research study (22).
Talk to Your Doctor About Hypoglycemia Treatments
The only definitive way to understand if you have hypoglycemia is to monitor your blood sugar with a blood glucose meter. This small machine is designed to take a small amount of blood by making a tiny puncture in the finger. A doctor may advise that you use a continuous glucose monitor to monitor your glucose levels throughout the day.
Follow your healthcare provider’s advice and take medications as prescribed, including insulin and medical devices. Diabetes usually involves regular doctor visits every three months and foot and eye exams yearly.
Suppose you are newly diagnosed with either T1 or T2 diabetes. In that case, a diabetes educator can spend more time with you than your doctor can answer all your practical lifestyle and medical device questions. You will also be encouraged to meet with a nutritionist to learn about healthy food strategies according to your circumstances. Many of today’s insurance plans now cover these extra services for diabetic patients.
Once you’ve discussed your treatment options, you can start talking about medical cannabis with your doctor. Nonetheless, cannabis should not be used as a substitute for other types of doctor-prescribed medications. It’s also important to consider that certain cannabis products, such as those containing THC, may trigger side effects like the munchies causing more food (including carbohydrate) intake.
Complementary Treatments Worth Discussing with Your Doctor
A handful of healing resources are available when treating low blood pressure. Otherwise known as “complementary medicine,” “complementary and alternative medicine,” or “complementary therapies,” these methods are aimed at strengthening the body’s natural healing powers.
The American Diabetes Association recommends that patients with hypoglycemia follow the “15-15 rule”, which includes the following rules:
- Eat or drink 15 grams of carbs for a blood sugar surge
- Check your blood sugar after 15 minutes
- If the blood sugar reading is still less than 70 mg/dL, consume an additional 15 grams of carbs
- Repeat the process until your blood sugar reads 70 mg/dL or higher (8)
Alternative treatment recommendations that may boost the body and mind include acupuncture, aromatherapy, Ayurvedic medicine, Chinese medicine, dietary supplements, guided imagery, and relaxation therapy. Some dietary supplements, including nicotinamide, vitamin E, vanadium, and chromium magnesium, may also help to regulate blood sugar levels (5).
You may also blend cannabis as complementary medicine into your health and wellness routine. Remember that although medical marijuana and other complementary medicines can prove beneficial for you or a loved one with an eating disorder, it’s important that you continue using any medication(s), devices, and follow-ups that your doctor prescribes.
Note: The content on this page is for informational purposes only and is not intended to be professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided. Always consult a physician before making any decision on the treatment of a medical condition.
1. The American Alliance of Medical Cannabis . (n.d.). Diabetes. AAMC: Diabetes – treatment with cannabis. Retrieved January 23, 2023, from http://www.letfreedomgrow.com/cmu/diabetes_5.htm
2. Centers for Disease Control and Prevention. (2021, August 10). Insulin resistance and diabetes. Centers for Disease Control and Prevention. Retrieved January 23, 2023, from https://www.cdc.gov/diabetes/basics/insulin-resistance.html#:~:text=Blood%20sugar%20enters%20your%20bloodstream,blood%20sugar%20for%20later%20use
3. Centers for Disease Control and Prevention. (2021, March 25). How to treat low blood sugar (hypoglycemia). Centers for Disease Control and Prevention. Retrieved January 23, 2023, from https://www.cdc.gov/diabetes/basics/low-blood-sugar-treatment.html
4. Centers for Disease Control and Prevention. (2022, September 30). Coexisting conditions and complications. Centers for Disease Control and Prevention. Retrieved January 23, 2023, from https://www.cdc.gov/diabetes/data/statistics-report/coexisting-conditions-complications.html
5. Costello, R. B., Dwyer, J. T., & Bailey, R. L. (2016). Chromium supplements for glycemic control in type 2 diabetes: Limited evidence of effectiveness. Nutrition Reviews, 74(7), 455–468. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5009459/
6. Endocrine Society. (2022, March 31). Hypoglycemia. Endocrine Society. Retrieved January 23, 2023, from https://www.endocrine.org/patient-engagement/endocrine-library/hypoglycemia
7. Gruden, G., Barutta, F., Kunos, G., & Pacher, P. (2015). Role of the endocannabinoid system in diabetes and diabetic complications. British Journal of Pharmacology, 173(7), 1116–1127. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4941127/
8. Hypoglycemia (low blood glucose). Hypoglycemia (Low Blood Glucose) | ADA. (n.d.). Retrieved January 23, 2023, from https://diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/hypoglycemia
9. Jadoon, K. A., Ratcliffe, S. H., Barrett, D. A., Thomas, E. L., Stott, C., Bell, J. D., O’Sullivan, S. E., & Tan, G. D. (2016). Efficacy and safety of Cannabidiol and Tetrahydrocannabivarin on glycemic and lipid parameters in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled, parallel group pilot study. Diabetes Care, 39(10), 1777–1786. https://pubmed.ncbi.nlm.nih.gov/27573936/
10. Jadoon, K. A., Tan, G. D., & O’Sullivan, S. E. (2017). A single dose of cannabidiol reduces blood pressure in healthy volunteers in a randomized crossover study. JCI Insight, 2(12). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5470879/
11. Joel Thome, P. D. (2018, October 16). Addressing hypoglycemic emergencies. U.S. Pharmacist – The Leading Journal in Pharmacy. Retrieved January 23, 2023, from https://www.uspharmacist.com/article/addressing-hypoglycemic-emergencies
12. Krzyżewska, A., Baranowska-Kuczko, M., Mińczuk, K., & Kozłowska, H. (2021). Cannabinoids—a new perspective in adjuvant therapy for pulmonary hypertension. International Journal of Molecular Sciences, 22(18), 10048. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8472313/
13. Mayo Foundation for Medical Education and Research. (2022, May 4). Hypoglycemia. Mayo Clinic. Retrieved January 23, 2023, from https://www.mayoclinic.org/diseases-conditions/hypoglycemia/symptoms-causes/syc-20373685
14. Mayo Foundation for Medical Education and Research. (2022, May 6). Diabetic hypoglycemia. Mayo Clinic. Retrieved January 23, 2023, from https://www.mayoclinic.org/diseases-conditions/diabetic-hypoglycemia/diagnosis-treatment/drc-20371529
15. NHS. (2020). Low blood sugar (hypoglycaemia). NHS choices. Retrieved January 23, 2023, from https://www.nhs.uk/conditions/low-blood-sugar-hypoglycaemia/#:~:text=A%20low%20blood%20sugar%20level%20without%20diabetes&text=not%20eating%20(fasting)%20or%20malnutrition,kidneys%2C%20adrenal%20glands%20or%20heart
16. Penner, E. A., Buettner, H., & Mittleman, M. A. (2013). The impact of marijuana use on glucose, insulin, and insulin resistance among us adults. The American Journal of Medicine, 126(7), 583–589. https://pubmed.ncbi.nlm.nih.gov/23684393/
17. Porr, C. J., Rios, P., Bajaj, H. S., Egan, A. M., Huot, C., Batten, R., Bishop, L., Ryan, D., Davis, E., Darvesh, N., Rahman, A., Asghari, S., Acheampong, L., & Tricco, A. C. (2020). The effects of recreational cannabis use on glycemic outcomes and self-management behaviours in people with type 1 and type 2 diabetes: A rapid review. Systematic Reviews, 9(1). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7433109/
18. Rock, E. M., Limebeer, C. L., Pertwee, R. G., Mechoulam, R., & Parker, L. A. (2021). Therapeutic potential of cannabidiol, cannabidiolic acid, and cannabidiolic acid methyl ester as treatments for nausea and vomiting. Cannabis and Cannabinoid Research. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8380783/
19. Rohbeck, E., Eckel, J., & Romacho, T. (2021). Cannabinoid receptors in metabolic regulation and diabetes. Physiology, 36(2), 102–113. https://journals.physiology.org/doi/full/10.1152/physiol.00029.2020?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
20. Severe hypoglycemia linked to increased risk of death in people with diabetes. Johns Hopkins Bloomberg School of Public Health. (2017, March 10). Retrieved January 23, 2023, from https://publichealth.jhu.edu/2017/severe-hypoglycemia-linked-to-increased-risk-of-death-in-people-with-diabetes
21. Walsh, K. B., McKinney, A. E., & Holmes, A. E. (2021). Minor cannabinoids: Biosynthesis, molecular pharmacology and potential therapeutic uses. Frontiers in Pharmacology, 12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8669157/
22. Xu, D. H., Cullen, B. D., Tang, M., & Fang, Y. (2020). The effectiveness of topical cannabidiol oil in symptomatic relief of peripheral neuropathy of the lower extremities. Current Pharmaceutical Biotechnology, 21(5), 390–402. https://pubmed.ncbi.nlm.nih.gov/31793418/