Cirrhosis and Medical Cannabis
Key Takeaways: Medical Cannabis for Cirrhosis
Research suggests cannabinoids, particularly CBD, found in cannabis may reduce inflammation, improve liver health, and relieve symptoms for cirrhosis patients. However, THC, another cannabis compound, may have less favorable effects on liver inflammation and fibrosis. Understanding the role of the endocannabinoid system in liver function is crucial, as it influences the outcome of liver diseases like cirrhosis.
Various cannabis preparations, such as edibles, capsules, tinctures, and patches, offer controlled dosing options. Complementary therapies like massage, meditation, and dietary supplements may also benefit cirrhosis patients alongside conventional medical treatments. It’s essential to consult with a healthcare professional before considering medical cannabis as a complementary treatment for cirrhosis.
The Science Behind Medical Cannabis for Cirrhosis
- Cirrhosis Causes and Complications
- Cirrhosis Treatment: Can Cannabinoids Provide Relief?
- The Role of the Endocannabinoid System in Treating Cirrhosis
- What Preparations of Cannabis are Best for Cirrhosis?
- Talk to Your Doctor About Medical Cannabis
The human body contains 79 organs, with the liver being the largest solid internal organ, as well as one of the most important (10). It carries out more than 500 vital functions and therefore liver damage caused by cirrhosis or other liver diseases pose a serious threat to overall health (8).
Cirrhosis is a late-stage liver disease that occurs when scar tissue irreversibly replaces healthy liver tissue. Since an estimated one in 400 adults in the U.S. are believed to suffer from cirrhosis, it goes without saying that this disease creates a significant dent on the lives of many as well as the healthcare sector (3).
Most patients with cirrhosis experience permanent damage, which will impact liver function. When the healthy liver cells become injured, they will usually become inflamed and/or die. Afterward, the cell repairs itself, and scar tissue forms.
Blood flow in the liver then becomes blocked by the scar tissue, which effectively hinders the liver’s ability to process nutrients, drugs, natural toxins, and hormones. Excess scar tissue also minimizes protein production and restricts the production of other liver-made substances.
As time progresses, cirrhosis completely disrupts the liver from doing its job, causing multiple serious health problems and eventually meaning that a patient’s life will be at risk. In fact, cirrhosis results in approximately 26,000 annual deaths in the U.S. and it is the seventh leading cause of death among people aged 25-65.
With many cirrhosis patients having exhausted their existing treatment options with little relief, there’s no wonder why scientists and doctors alike are exploring alternative methods of treatment. Unfortunately for advanced cirrhosis patients, there is often little hope for a liver transplant due to a long waitlist and specific qualifications.
Cannabis in certain circumstances has been shown to enhance liver health, reduce inflammation, and enhance the immune system. There is some conflicting preclinical and clinical evidence, but the big picture now overall looks favorable in lower doses and with medication interactions accounted for. Taking this into account, it’s certainly worth learning more about using this natural remedy in cases of cirrhosis.
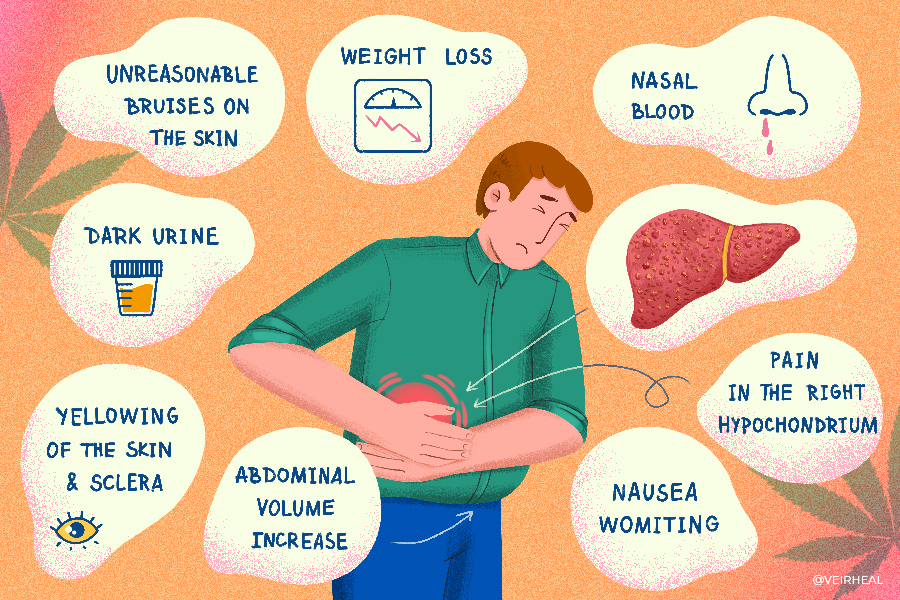
Cirrhosis Causes and Complications
Cirrhosis impacts the lives of approximately one in every 200 adults aged between 45 and 54 — the age demographic that tends to suffer the most from cases of cirrhosis. The seriousness of liver cirrhosis should not be ignored, because when it reaches a cirrhotic state, the depleted liver can no longer be repaired and needs to be replaced.
When you have irreversible damage to the liver, you are likely to be faced with the prognosis of possible liver cancer, serious blood, brain, and liver-related complications, liver failure, and eventual death. Numerous factors may increase the chances of developing cirrhosis, such as:
- Autoimmune liver disease (autoimmune hepatitis, primary biliary cirrhosis or primary sclerosing cholangitis)
- Alcohol consumption
- Chronic hepatitis B
- Chronic hepatitis C
- Diabetes
- Fatty liver disease (non-alcoholic steatohepatitis)
- Genetic and hereditary conditions
- Hemochromatosis
- HIV and shared IV needle use, or unprotected sex
- Metabolic syndrome
- Medication and toxin buildup
- Obesity
- Viral infections
- Wilson’s disease
Since the liver’s role involves maintaining various critical functions within the body, damage to the liver or changes to its functions can result in the body becoming severely harmed in numerous ways.
Cirrhosis Treatment: Can Cannabinoids Provide Relief?
The liver’s essential psychological functions are critical not only for digestive disorders but also, for metabolism, blood and brain function, immunity, and human survival. Aside from regulating blood clotting and the production/processing of bile, glycogen, special proteins like plasma, hemoglobin, and ammonia-derived urea — the liver also regulates amino acid levels, detoxifies the blood, and flushes out bilirubin.
Most doctors tend to prescribe a necessary plethora of medications and treatments for cirrhosis management, which are all very important, there’s also new but still early scientific evidence to support the potentially supplemental use of medical cannabis for cirrhosis, not to mention other types of liver conditions.
Marijuana has natural antioxidant and anti-inflammatory powers that could ease liver pain and not cause further hepatic fibrosis. Plus, clinical trials and studies have shown that cannabinoids may possess the capability to be used with success in the treatment of gut and liver diseases.
One specific cannabinoid, cannabidiol (CBD), may be one of the most impressive in terms of improving digestive health. The non-psychotropic cannabinoid has been shown to exhibit antioxidant, anti-inflammatory, and hepatoprotective effects in clinical studies.
CBD also has anti-fibrosis qualities that make it useful for reducing collagen secretion that causes fibrosis (15). It can also reverse changes in the liver associated with alcohol-induced injury plus high-fat diet, and in situations of binge drinking (7, 14).
CBD has been highlighted for its therapeutic potential in relieving the inflammatory changes and fatty degeneration of numerous chronic liver diseases. One study published in the World Journal of Hepatology, researchers found a lower prevalence of nonalcoholic fatty liver disease (NAFLD) among cannabis consumers (2).
A 2019 systematic review and meta-analysis also concurs with the World Journal of Hepatology study (6). They looked at all of the conflicting research and concluded that “Marijuana use did not increase the prevalence or progression of hepatic fibrosis in HCV and HCV–HIV-coinfected patients. On the contrary, we noted a reduction in the prevalence of Nonalcoholic fatty liver disease (NAFLD) in marijuana users. Future studies are needed to further understand the therapeutic impact of cannabidiol-based formulations in the management of NAFLD.”
In the FDA trials for EpidiolexⓇ (very high-dose pharmaceutical CBD), there was concern for elevated liver enzymes which indicated liver injury. However, this was more likely attributable to the anti-seizure drugs (e.g. clobazam, valproate) that the patients were still taking since CBD raised the levels of those drugs. When either drug or CBD was reduced, the liver injury was reversed in over 2/3rds of patients (5).
On the other hand, THC may actually increase the growth of hepatic myofibroblasts and stellate cells because of its CB1 receptor activation. Furthermore, the psychoactive mind-altering compound reduces apoptosis (cell death), meaning that the cannabinoid may have profibrotic and hepatic inflammatory properties.
The Role of the Endocannabinoid System in Treating Cirrhosis
The endocannabinoid system (ECS) is responsible for maintaining homeostasis. Two unique cannabinoid receptors, CB1 and CB2, represent an important part of the ECS. Found scattered throughout the body and brain, cannabinoid receptors act directly and indirectly on CB1 and CB2 receptors.
CB1 is mostly expressed in the brain and in the periphery, whereas CB2 has been identified in the brain, bone, hematopoietic system, periphery, liver, pancreas, and immune cells. CB1 and CB2 receptors have been highlighted in various pathological processes, thus thrusting this scope of medical cannabis research to the forefront of the conversation about cirrhosis treatments.
The endocannabinoid system has been shown to influence the outcome of liver disease, and especially in cases of cirrhosis. Scientists have learned that CB2 receptors play a key part in treating chronic and acute liver injury, including liver reperfusion injury and hepatic encephalopathy pertaining to acute liver failure (11).
CB1 and CB2 agonism and antagonism have been explored in clinical studies and trials on cirrhosis. Mallat et al. taught us that CB1 and CB2 receptors are upregulated in cirrhotic liver samples. CB1 activation promotes fibrogenesis, while CB2 activation reduces inflammation and impedes progression to fibrosis (9).
A systematic review found that CB2 deficiency led to prolonged survival of liver fibrogenic cells, thus amplifying fibrosis with increased deposition of fibrotic tissue (1). Researchers have also demonstrated that CB2 boosts the regenerative response after acute liver injury (9).
A study, titled, “The Role of Cannabinoids in the Setting of Cirrhosis” revealed that, “CB1 antagonism has also demonstrated vascular effects in patients with cirrhosis, causing an increase in arterial pressure and vascular resistance as well as a decrease in mesenteric blood flow and portal pressure, thereby preventing ascites (4).” Ascites is fluid buildup between the abdominal lining and the abdominal organs. Ascites is often controlled by sodium and fluid restriction and may need to be manually extracted by a doctor.
The 2019 review data suggests that THC may be detrimental to hepatic inflammation and fibrosis because it acts on CB1, while CBD acts on other receptors and targets that may be helpful instead. THC also acts on CB2, which would be helpful if it did not also activate CB1 (6). So, if there were a cannabinoid that acted specifically on CB2, combined with CBD, their combined anti-inflammatory effects would be most beneficial and could help with liver cirrhosis complications like hepatic encephalopathy (1).
The 2019 review also explains in detail how CB1 receptor activation is harmful in liver inflammation, while CB2 activation is better (6). “CB1 receptor activation is associated with profibrogenic effects with increased expression of transforming growth factor β−1, increased stellate cell production, and decreased apoptosis leading [sic] higher rates of hepatic fibrogenesis. In addition, it is also associated with decreased production of adiponectin, an adipokine with antifibrotic properties in animal models. Finally, CB1 receptor also promotes hepatic fatty-acid production and participates in diet-related obesity.
On the contrary, activation of CB2 receptors in mice has been associated with antifibrogenic and anti-inflammatory properties such as suppression of macrophage function of antigen presentation, inhibits chemokine production by human B cells, decreases macrophage nitric-oxide production, suppresses cytotoxic T-cell proliferation, and favorably regulates tumor necrosis factor, interleukin-1, and interferon gamma production by mononuclear cells. Overall, stimulation of CB2 receptor results in reduction of oxidative stress and retards cell death.”
What Preparations of Cannabis are Best for Cirrhosis?
One of the main perks associated with medical cannabis consumption is the diversity in terms of product options. Various CBD preparations are available for cirrhosis patients, many of which allow for controlled dosing and discretion.
Examples of some effective cannabis preparations with desirable bioavailability include:
- Edibles
- Pills, Capsules, and Tablets
- Cannabis Powder/Dissolvable Cannabis
- Transdermal Patches
- Vapes
- Tinctures
Talk to Your Doctor About Medical Cannabis
To better understand exactly what type of cirrhosis you are dealing with, as well as to determine whether or not your cramps are associated with a physiological condition, your doctor or healthcare practitioner may conduct a medical examination.
After a diagnosis, you can discuss the prospect of using cannabis-based treatment options with a doctor. However, it’s important to note that cannabis should not be used as a substitute for other types of doctor-prescribed medications.
Complementary and alternative medicine (CAM) is an umbrella term that encompasses a wide scope of integrative and holistic healing resources aimed at preventing or treating illness/disease, as well as promoting overall health and well-being. When someone with cirrhosis introduces complementary medicine into their daily routine, the road to recovery could be much smoother.
Examples of complementary medicine include massage, meditation, biofeedback, tai chi, reiki, music therapy, guided imagery and dietary supplements. Consuming a low-THC, high-CBD strain could enhance the outcome of these techniques, since cannabis is a powerful anxiolytic, analgesic, and anti-inflammatory (12).
Studies have also shown that a substance contained in milk thistle (silymarin) may shield the liver from damage caused by alcohol, toxins, viruses, and certain medications like acetaminophen (Tylenol). (World Journal of Hepatology) (13).
While these complementary therapies can prove beneficial, it’s important that you continue using any medication(s) and treatments that are prescribed by your doctor.
Note: The content on this page is for informational purposes only and is not intended to be professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided. Always consult a physician before making any decision on the treatment of a medical condition.
1. Baldassarre, M., Giannone, F. A., Napoli, L., Tovoli, A., Ricci, C. S., Tufoni, M., & Caraceni, P. (2013). The endocannabinoid system in advanced liver cirrhosis: Pathophysiological implication and future perspectives. Liver International, 33(9), 1298–1308. https://pubmed.ncbi.nlm.nih.gov/23890208/
2. Choi, C. J., Weiss, S. H., Nasir, U. M., & Pyrsopoulos, N. T. (2020). Cannabis use history is associated with increased prevalence of ascites among patients with nonalcoholic fatty liver disease: A nationwide analysis. World Journal of Hepatology, 12(11), 993–1003. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7701971/
3. Cirrhosis of the liver: What is it, symptoms, causes & stages. Cleveland Clinic. (n.d.). Retrieved September 15, 2022, from https://my.clevelandclinic.org/health/diseases/15572-cirrhosis-of-the-liver
4. Dibba, P., Li, A., Cholankeril, G., Iqbal, U., Gadiparthi, C., Khan, M., Kim, D., & Ahmed, A. (2018). The role of cannabinoids in the setting of cirrhosis. Medicines, 5(2), 52. https://pubmed.ncbi.nlm.nih.gov/29890719/
5. Epidiolex (cannabidiol) oral solution – food and drug administration. (n.d.). Retrieved September 15, 2022, from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210365lbl.pdf
6. Farooqui, M. T., Khan, M. A., Cholankeril, G., Khan, Z., Mohammed Abdul, M. K., Li, A. A., Shah, N., Wu, L., Haq, K., Solanki, S., Kim, D., & Ahmed, A. (2019). Marijuana is not associated with progression of hepatic fibrosis in liver disease: A systematic review and meta-analysis. European Journal of Gastroenterology & Hepatology, 31(2), 149–156. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6467701/
7. Jiang, X., Gu, Y., Huang, Y., Zhou, Y., Pang, N., Luo, J., Tang, Z., Zhang, Z., & Yang, L. (2021). CBD alleviates liver injuries in alcoholics with high-fat high-cholesterol diet through regulating NLRP3 inflammasome–pyroptosis pathway. Frontiers in Pharmacology, 12. https://www.frontiersin.org/articles/10.3389/fphar.2021.724747/full
8. Liver: Anatomy and functions. Johns Hopkins Medicine. (2019, November 19). Retrieved September 15, 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-anatomy-and-functions
9. Mallat, A., Teixeira-Clerc, F., Deveaux, V., Manin, S., & Lotersztajn, S. (2011). The endocannabinoid system as a key mediator during liver diseases: New insights and therapeutic openings. British Journal of Pharmacology, 163(7), 1432–1440. https://pubmed.ncbi.nlm.nih.gov/21457226/
10. Nunez, K. (2020, February 18). Largest organ in the body: Size, weight & interesting facts. Healthline. Retrieved September 15, 2022, from https://www.healthline.com/health/largest-organs-in-the-body
11. Parfieniuk, A., & Flisiak, R. (2008). Role of cannabinoids in Chronic liver diseases. World Journal of Gastroenterology, 14(40), 6109. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2761570/
12. Russo, E. (2008). Cannabinoids in the management of difficult to treat pain. Therapeutics and Clinical Risk Management, Volume 4, 245–259. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2503660/
13. Vargas-Mendoza, N. (2014). Hepatoprotective effect of Silymarin. World Journal of Hepatology, 6(3), 144. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3959115/#:~:text=Silymarin%20is%20an%20antioxidant%20that,%2C%20and%20anti%2Dfibrotic%20activities
14. Yang, L., Rozenfeld, R., Wu, D., Devi, L. A., Zhang, Z., & Cederbaum, A. (2014). Cannabidiol protects liver from binge alcohol-induced steatosis by mechanisms including inhibition of oxidative stress and increase in autophagy. Free Radical Biology and Medicine, 68, 260–267. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4112960/
15. Zurier, R. B., & Burstein, S. H. (2016). Cannabinoids, inflammation, and fibrosis. The FASEB Journal, 30(11), 3682–3689. https://www.researchgate.net/publication/305461086_Cannabinoids_inflammation_and_fibrosis