Medical Marijuana: is it a Possible Option for Darier’s Disease?
- How Medical Cannabis Helps the Skin
- Transient Receptor Potential Channels and Darier’s Disease
- Medical Cannabis for Darier’s Related Medical Conditions
- Medical Cannabis Patients with Darier’s Disease: Important Considerations
- Understanding Darier’s Disease and Types
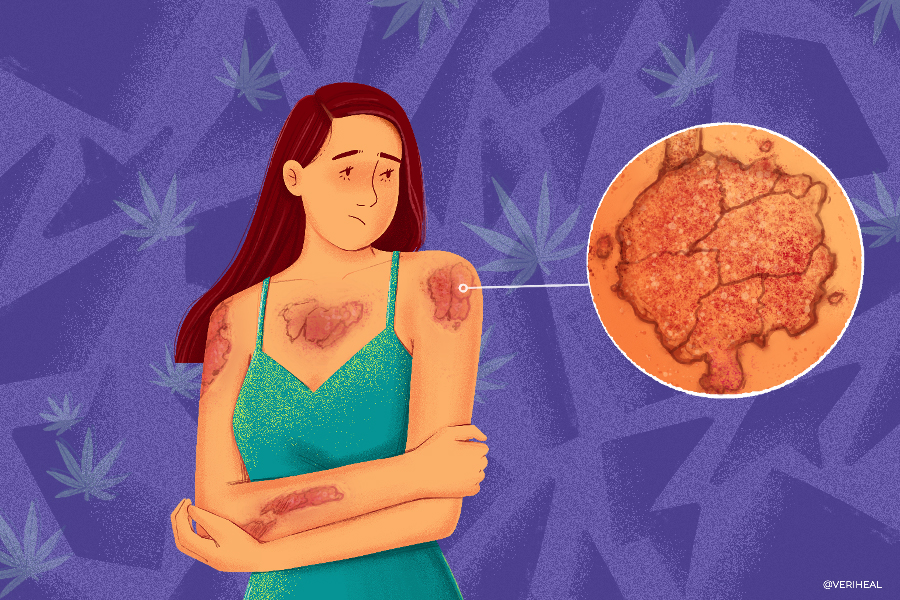
Darier’s disease (DD), also known as Darier-White disease, dyskeratosis follicularis, and keratosis follicularis, is a difficult genetic condition for those who have it. It typically shows up in adolescents or young adults and is characterized by periods of clear skin followed by flare-ups of wart-like blemishes on the body (35). Changes in humidity, heat, ultraviolet (UV) light, and friction or injuries to the skin can cause flare-ups (39).
DD is primarily characterized by hyperpigmented spots that are greasy and chronic itching called pruritus. Because the barrier of the skin is damaged, it can lead to bacterial infections of the skin. The pigmented spots are often greasy papules on the skin (1). Occasionally the papules or blisters can lead to lesions or skin ulcers.
Through a lot of research studies, medical cannabis has proven to be a strong potential treatment for a variety of skin conditions including acne, psoriasis, epidermolysis bullosa, skin cancer, and xeroderma pigmentosum.
We now know that treating the skin with cannabis, including Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD), begins with its ability to interact with our bodies partly due to the endocannabinoid system (ECS). The ECS is a bodily system that we all have. It consists of fat-based neurotransmitters called that are activated by cannabinoid receptors CB1 and CB2 that are found all over our bodies. These neurotransmitters, including anandamide (AEA) and 2-arachidonoylglycerol (2-AG), can be increased or decreased when the ECS is activated. This is responsible for a variety of processes in our body including modulating inflammation, how we perceive pain, and helping our body maintain its optimal temperature and operating state called homeostasis.
How Medical Cannabis Helps the Skin
There is a lot of current research that suggests that the skin contains large levels of endocannabinoids and cannabinoid receptors. Research shows that the main type of skin cell called keratinocytes contains both CB1 and CB2 receptors (3). This is important because, in patients with DD, the keratinocytes are unable to properly stick together, which causes faults in the skin barrier and can allow infections (9) (12).
Cannabinoids have also been shown to exert immunosuppressive properties by blocking leukocyte proliferation, inducing cellular death of T-cells and macrophages, and reducing the secretion of pro-inflammatory cytokines (30). A case study focusing on a patient with DD that was complicated by a dangerous herpes simplex virus worsened by the ability of cannabinoids to reduce immune system function to fight off the infection. Cannabinoids in this case study were shown to impair the immune system’s response to the proliferating herpes virus and actually mediated the reactivation of the virus. Thus cannabinoid abuse, in this case, resulted in a life-threatening infection by decreasing immune cell function. These results can also be seen in cases of the herpes simplex virus that were not complicated by DD (13).
There are also cannabinoid receptors in melanocytes (cells that produce melanin or pigment) as well as in nerve fibers of the skin, sweat glands, sebaceous glands that produce oil, and hair follicles (3). Research from The Journal of Clinical Investigation shows that CBD is good at inhibiting or slowing down excess oil production in sebocytes (oil glands of the skin) as well as causing the irregular cells the ability to die, which decreases infections relating to acne in the skin (40). CBD’s ability to impact sebocytes may also be important for DD and other skin disorders that result from excess oil production. CBD also helps moisturize the skin which reduces itching.
Transient Receptor Potential Channels & Darier’s Disease
In addition to targeting cannabinoids receptors of the skin, endocannabinoids also target the receptors of transient receptor potential (TRP) channels (3). TRP receptors are typically located on sensory nerve fibers in the body, including on the skin and in joint tissues (21). They are also responsible for the formation and maintenance of the skin barrier and serve immunological functions as well as help reduce inflammation in the skin. TRP receptors are a major target for cannabinoid research in DD and calcium is important for normal functions of and promoting changes in keratinocytes in various layers of the skin.
Research shows that activation of TRPV receptors and TRPC6 receptors play a role in calcium influx in keratinocytes (12) (23). TRP receptors also play a role in reducing itching as well as pain (12). Some researchers also believe that TRPC1 receptors play a role because they show an increased expression in DD patients. They believe that increased TRPC1 reduces cellular death in abnormal keratinocytes, or that maybe TRPC1 receptors are simply upregulated as a compensation method for the decreased functionality of SERCA2 in these patients (24) (25).
Medical Cannabis for Darier’s Related Medical Conditions
Darier’s disease has been linked to other medical conditions that may potentially be eased by medical cannabis. These conditions include (31):
- Epilepsy
- ADHD
- Anxiety
- Depression
- Melanoma (Skin cancer)
- Salivary gland disorders
- Kidney Diseases
- Heart failure (2)
Medical Cannabis Patients with Darier’s Disease: Important Considerations
Despite all the research relating to keratinocytes, TRP receptors, and sebaceous glands regarding the activation of the endocannabinoid system, dermatologists do not yet have enough data to recommend using cannabis and cannabinoid topical products for the skin (18). Utilizing these products for Darier’s disease is at your own risk.
Before beginning the use of medical cannabis, including topical lotions and creams, it is important to reach out to your dermatologist that is responsible for treating your case. Medical marijuana can interact with other medications you may be taking and may cause issues with some dermatological procedures.
It is important to note that patients who have DD have a higher risk for heart failure and other heart problems because of the genetic issues this population has to calcium regulation in the body (2). Side effects of cannabis use can also increase the risk of tachycardia and other heart issues. It also includes the possibility of reactivating latent HSV and causing a more severe infection due to cannabis’ immune-suppressing effects. Be advised that oral retinoids are the mainstay of treatment in Darier’s disease, and be sure to follow the advice of your doctor.
If you do decide that you would like to try using medical cannabis for Darier’s disease, it is important to understand how to purchase safe cannabinoid products from a dispensary. Please check out our CBD guide for more information on how to pick out safe products.
Understanding Darier’s Disease & Types
Darier’s disease or keratosis follicularis is considered a genetic skin disorder. It is caused by mutations in the sarcoplasmic/endoplasmic reticulum calcium ATPase gene (ATP2A2) that is responsible for producing an enzyme called SERCA2 (35). This enzyme is important because it helps control the levels of calcium ions inside the cells in our body. Calcium is essential for cells to function properly and the SERCA2 enzyme allows calcium to pass in and out of cells in response to cellular signals.
In patients with Darier’s disease, they do not produce enough of the SERCA2 enzyme that is needed to control calcium. Strangely, this imbalance shows up as blemishes in the skin even though SERCA2 is used throughout our bodies (35). Some researchers believe that this genetic mutation shows up in the skin because skin cells do not have a backup enzyme to help influence calcium moving in between the cells. Keratocytes, skin cells that are responsible for producing keratin, typically stick together during the formation of the skin barrier via structures called desmosomes, but these structures do not work assemble properly if there is not enough calcium, which allows for defects in the skin that can let in bacteria or herpes simplex viruses (9).
There are several subtypes of Darier’s, most very rare, including, but not limited to (1):
Classic Darier’s Disease
The level symptoms of classic Darier’s can be mild where symptoms are difficult to notice, or they can be severe depending on the individual (9). The severity of the disease can change over time as many patients experience flare-ups that cause the skin symptoms to worsen. The papules are usually scaly and greasy and can affect oily areas of the face, the scalp, neck, central chest, the back, and can appear in skin folds such as the groin, under the breasts, and in the armpits. The papules may form a yellow crust, like seborrheic dermatitis, a type of eczema.
Segmental or Linear Darier’s Disease
This form of Darier’s is characterized by blemishes on localized areas of the skin, instead of being widespread as in other forms of the disease (39). Some patients with this form also experience abnormalities in their nails, but unlike the classic form, these abnormalities only occur on one side of the body.
The linear form is also not inherited and is due to acquired mutations in the DNA (39). This means that genetic changes from environmental factors such as UV damage, exposure to harsh chemicals, or carcinogens are to blame rather than being born with mutations of the ATP2A2 gene.
Acrokeratosis Verruciformis of Hopf
This type of Darier’s disease is caused by an inherited defect in the ATP2A2 gene (8). This inherited disorder occurs when a parent passes on a defective ATP2A2 gene to a child. The child needs to only have one ATP2A2 inherited defect to show symptoms, thus has a 1 and 2 chance of inheriting it if a parent also has acrokeratosis verruciformis of Hopf.
It is characterized by grouped or isolated papules on the knees, elbows, and forearms. Patients can also have pits on the palms of the hands and the soles of their feet (8). These patients also tend to have deformities of their fingernails and toenails where the nails look pearly white or have vertical ridges.
Acral Hemorrhagic Darier’s Disease
The Acral hemorrhagic form of Darier’s is extremely rare with only around 20 cases being reported as of 2017 (14). It is characterized by red and bloody-looking blisters intermixed with the typical papules of Darier’s disease in severe cases.
Note: Veriheal does not intend to give this as professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided on this page. Always consult a physician before making any decision on the treatment of a medical condition.
1. Alsharif, S. H., Alesa, D., & Baabdullah, A. (2020). Type 1 segmental Darier Disease: Case report and discussion of the treatment options. Case Reports in Dermatology, 12(3), 159–167. https://www.karger.com/Article/FullText/509177
2. Bachar-Wikstrom, E., Curman, P., Ahanian, T. et al. Darier disease is associated with heart failure: a cross-sectional case-control and population based study. Sci Rep 10, 6886 (2020). https://www.nature.com/articles/s41598-020-63832-9
3. Baswan, S. M., Klosner, A. E., Glynn, K., Rajgopal, A., Malik, K., Yim, S., & Stern, N. (2020). Therapeutic Potential of Cannabidiol (CBD) for Skin Health and Disorders. Clinical, cosmetic and investigational dermatology, 13, 927–942. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7736837/
4. Bíró, T., Tóth, B. I., Marincsák, R., Dobrosi, N., Géczy, T., & Paus, R. (2007). TRP channels as novel players in the pathogenesis and therapy of itch. Biochimica Et Biophysica Acta (BBA) – Molecular Basis of Disease, 1772(8), 1004–1021. https://www.sciencedirect.com/science/article/pii/S0925443907000774
5. Boudaka, A., Al-Yazeedi, M., & Al-Lawati, I. (2020). Role of Transient Receptor Potential Vanilloid 4 Channel in Skin Physiology and Pathology. Sultan Qaboos University medical journal, 20(2), e138–e146. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7328835/
6. Caterina, M., & Pang, Z. (2016). TRP channels in Skin Biology and Pathophysiology. Pharmaceuticals, 9(4), 77. https://www.mdpi.com/1424-8247/9/4/77
7. Chung, J., Kim, J. Y., Gye, J., Namkoong, S., Hong, S. P., Park, B. C., & Kim, M. H. (2011). A Case of Familial Comedonal Darier’s Disease. Annals of dermatology, 23(Suppl 3), S398–S401. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3276807/
8. DermNet NZ. (n.d.). Acrokeratosis verruciformis of Hopf. Acrokeratosis verruciformis of Hopf. Retrieved January 13, 2022, from https://dermnetnz.org/topics/acrokeratosis-verruciformis-of-hopf
9. DermNet NZ. (n.d.). Darier disease. Retrieved January 13, 2022, from https://dermnetnz.org/topics/darier-disease
10. Dobrosi, N., Tóth, B. I., Nagy, G., Dózsa, A., Géczy, T., Nagy, L., Zouboulis, C. C., Paus, R., Kovács, L., & Bíró, T. (2008). Endocannabinoids enhance lipid synthesis and apoptosis of human sebocytes via cannabinoid receptor‐2‐mediated signaling. The FASEB Journal, 22(10), 3685–3695. https://faseb.onlinelibrary.wiley.com/doi/10.1096/fj.07-104877
11. Eagleston, L. R., Kalani, N. K., Patel, R. R., Flaten, H. K., Dunnick, C. A., & Dellavalle, R. P. (2018). Cannabinoids in dermatology: A scoping review. Dermatology Online Journal, 24(6). https://escholarship.org/uc/item/7pn8c0sb
12. Elsholz, F., Harteneck, C., Muller, W. et al. Calcium — a central regulator of keratinocyte differentiation in health and disease. Eur J Dermatol 24, 650–661 (2014). https://link.springer.com/article/10.1684/ejd.2014.2452
13. Fischer-Stenger, K., Updegrove, A. W., & Cabral, G. A. (1992). Delta 9-tetrahydrocannabinol decreases cytotoxic T lymphocyte activity to herpes simplex virus type 1-infected cells. Proceedings of the Society for Experimental Biology and Medicine. Society for Experimental Biology and Medicine (New York, N.Y.), 200(3), 422–430. https://pubmed.ncbi.nlm.nih.gov/1319584/
14. Flores-Terry, M. Á., García-Arpa, M., Llamas-Velasco, M., Mendoza-Chaparro, C., & Ramos-Rodríguez, C. (2017). Acral hemorrhagic Darier disease. Actas Dermo-Sifiliográficas (English Edition), 108(7). https://www.actasdermo.org/en-acral-hemorrhagic-darier-disease-articulo-S1578219017301907
15. Fusi, C., Materazzi, S., Minocci, D., Maio, V., Oranges, T., Massi, D., & Nassini, R. (2014). Transient receptor potential vanilloid 4 (TRPV4) is downregulated in keratinocytes in human non-melanoma skin cancer. Journal of Investigative Dermatology, 134(9), 2408–2417. https://www.sciencedirect.com/science/article/pii/S0022202X15369700
16. Garbutcheon‐Singh, K. B., & Smith, S. D. (2021). Cannabinoids interaction with transient receptor potential family and implications in the treatment of rosacea. Dermatologic Therapy. https://onlinelibrary.wiley.com/doi/10.1111/dth.15162
17. Gupta, A. K., & Talukder, M. (2021). Cannabinoids for skin diseases and hair regrowth. Journal of Cosmetic Dermatology, 20(9), 2703–2711. https://onlinelibrary.wiley.com/doi/10.1111/jocd.14352
18. Hashim, P. W., Cohen, J. L., Pompei, D. T., & Goldenberg, G. (2017). Topical cannabinoids in dermatology. Cutis, 100(1), 50–52. https://cdn.mdedge.com/files/s3fs-public/Document/July-2017/CT100001050.PDF
19. Kupczyk, P., Reich, A., & Szepietowski, J. C. (2009). Cannabinoid system in the skin – a possible target for future therapies in dermatology. Experimental Dermatology, 18(8), 669–679. https://onlinelibrary.wiley.com/doi/10.1111/j.1600-0625.2009.00923.x
20. Liszewski, W., & Farah, R. S. (2017). Response to: “the role of cannabinoids in dermatology.” Journal of the American Academy of Dermatology, 77(3). https://www.jaad.org/article/S0190-9622(17)31770-X/fulltext
21. Lowin, T., & Straub, R. H. (2015). Cannabinoid-based drugs targeting CB1 and TRPV1, the sympathetic nervous system, and arthritis. Arthritis research & therapy, 17(1), 226. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4561168/
22. Milando, R., & Friedman, A. (2018). Cannabinoids: Potential role in inflammatory and neoplastic skin diseases. American Journal of Clinical Dermatology, 20(2), 167–180. https://link.springer.com/article/10.1007%2Fs40257-018-0410-5
23. Müller, M., Essin, K., Hill, K., Beschmann, H., Rubant, S., Schempp, C. M., Gollasch, M., Boehncke, W. H., Harteneck, C., Müller, W. E., & Leuner, K. (2008). Specific TRPC6 channel activation, a novel approach to stimulate keratinocyte differentiation. The Journal of biological chemistry, 283(49), 33942–33954. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2662218/
24. Pani, B., Cornatzer, E., Cornatzer, W., Shin, D. M., Pittelkow, M. R., Hovnanian, A., Ambudkar, I. S., & Singh, B. B. (2006). Up-regulation of transient receptor potential canonical 1 (TRPC1) following sarco(endo)plasmic reticulum Ca2+ ATPase 2 gene silencing promotes cell survival: a potential role for TRPC1 in Darier’s disease. Molecular biology of the cell, 17(10), 4446–4458. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1635355/
25. Pani, B., & Singh, B. B. (2008). Darier’s disease: a calcium-signaling perspective. Cellular and molecular life sciences : CMLS, 65(2), 205–211. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2690644/
26. Pui-Yan Kwok, M. D. (2020, October 1). Keratosis follicularis (Darier disease). Background, Pathophysiology, Epidemiology. Retrieved January 13, 2022, from https://emedicine.medscape.com/article/1107340-overview
27. Ramot, Y., Oláh, A., & Paus, R. (2018). Cover image: Neuroendocrine treatment of inherited keratin disorders by cannabinoids? British Journal of Dermatology, 178(6), 1469–1469. https://onlinelibrary.wiley.com/doi/10.1111/bjd.16570
28. Rao, G. K., & Kaminski, N. E. (2006). Cannabinoid-mediated elevation of intracellular calcium: A structure-activity relationship. Journal of Pharmacology and Experimental Therapeutics, 317(2), 820–829. https://jpet.aspetjournals.org/content/317/2/820
29. Río, C. del, Millán, E., García, V., Appendino, G., DeMesa, J., & Muñoz, E. (2018). The endocannabinoid system of the skin. A potential approach for the treatment of Skin disorders. Biochemical Pharmacology, 157, 122–133. https://www.sciencedirect.com/science/article/abs/pii/S0006295218303484?via%3Dihub
30. Russo, R., Labate, L., Cozzani, E., Delfino, E., Bassetti, M., & Parodi, A. (2021). Kaposi-Juliusberg Varicelliform Eruption complicating Darier disease: May cannabinoid abuse be an underestimated risk factor?. Clinical case reports, 9(8), e04589. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8365399/
31. Sánchez Martínez, E. M., Moneva Léniz, L. M., Gegúndez Hernández, H., & Mateu Puchades, A. (2021). Darier Disease: A case series of 20 patients and review of the literature. Actas Dermo-Sifiliográficas (English Edition). https://www.actasdermo.org/en-darier-disease-a-case-series-articulo-S1578219021001566
32. Sulk, M., & Steinhoff, M. (2015). Role of TRP channels in skin diseases. TRP Channels as Therapeutic Targets, 293–323. https://www.sciencedirect.com/science/article/pii/B9780124200241000175
33. Tahamtan, A., Tavakoli-Yaraki, M., Rygiel, T. P., Mokhtari-Azad, T., & Salimi, V. (2016). Effects of cannabinoids and their receptors on viral infections. Journal of medical virology, 88(1), 1–12. https://pubmed.ncbi.nlm.nih.gov/26059175/
34. Tóth, K., Ádám, D., Bíró, T., & Oláh, A. (2019). Cannabinoid signaling in the skin: Therapeutic potential of the “c(ut)annabinoid” system. Molecules, 24(5), 918. https://www.mdpi.com/1420-3049/24/5/918
35. U.S. National Library of Medicine. (2021, April 7). Darier disease: Medlineplus Genetics. MedlinePlus. Retrieved January 13, 2022, from https://medlineplus.gov/genetics/condition/darier-disease/
36. Valdes-Rodriguez, R., B. Kaushik, S., & Yosipovitch, G. (2013). Transient receptor potential channels and dermatological disorders. Current Topics in Medicinal Chemistry, 13(3), 335–343. https://pubmed.ncbi.nlm.nih.gov/23432064/
37. V, S., S, S., B K, Y. D., N, R., T, P. K., R, P., & Krishnamurthy, Y. (2019). Spectrum of features in Darier’s disease: A case report with emphasis on differential diagnosis. Journal of oral biology and craniofacial research, 9(2), 215–220. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6562229/
38. Wang, J. F., Lederhandler, M. H., Brinster, N., & Soter, N. A. (2019). Vesiculobullous Darier Disease Symptomatically Responsive to Cetirizine. Journal of drugs in dermatology : JDD, 18(2), 213–214. https://jddonline.com/articles/vesiculobullous-darier-disease-symptomatically-responsive-to-cetirizine-S1545961619P0213X/
39. U.S. Department of Health and Human Services. (n.d.). Darier disease. Genetic and Rare Diseases Information Center. Retrieved January 19, 2022, from https://rarediseases.info.nih.gov/diseases/6243/darier-disease%20SERCA
40. Oláh, A., Tóth, B. I., Borbíró, I., Sugawara, K., Szöllõsi, A. G., Czifra, G., Pál, B., Ambrus, L., Kloepper, J., Camera, E., Ludovici, M., Picardo, M., Voets, T., Zouboulis, C. C., Paus, R., & Bíró, T. (2014). Cannabidiol exerts sebostatic and antiinflammatory effects on human sebocytes. The Journal of clinical investigation, 124(9), 3713–3724. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4151231/








