Can Medical Marijuana Help Digestive Disorder?
Medical Cannabis and Digestive Disorders: What You Need to Know
Medical cannabis presents a promising avenue for managing digestive disorders, providing relief for people grappling with conditions like inflammatory bowel disease (IBD), Crohn’s disease, and irritable bowel syndrome (IBS). One significant advantage lies in its capacity to alleviate symptoms commonly associated with these disorders, including abdominal pain, cramping, and nausea. By engaging with the body’s endocannabinoid system, cannabinoids found in cannabis can regulate gastrointestinal motility and inflammation, offering a potential source of comfort for those experiencing gastrointestinal distress.
Additionally, the anti-inflammatory properties inherent in medical cannabis can offer targeted relief for individuals grappling with inflammatory bowel diseases. Chronic inflammation within the digestive tract characterizes these conditions, resulting in tissue damage and exacerbation of symptoms. Through its modulation of inflammatory pathways, cannabis compounds like THC and CBD demonstrate the potential to mitigate inflammation, offering a glimmer of hope for patients seeking effective symptom management. Additionally, cannabis’s ability to stimulate appetite and reduce nausea can prove invaluable in addressing common side effects of medication or the disease process itself, potentially promoting better nutritional intake and overall well-being for those affected by digestive disorders. In essence, medical cannabis stands as a promising adjunctive therapy in the multifaceted management of digestive disorders, offering a natural approach to symptom relief and improved quality of life.
The Science Behind Medical Cannabis for Digestive Disorders
- Digestive Disorders: Signs, Symptoms and Types
- Digestive Disorders: Causes and Complications
- Digestive Disorders Treatment: Can Cannabinoids Provide Relief?
- The Role of the Endocannabinoid System in Treating Digestive Disorders
- What Preparations of Cannabis are Best for Digestive Disorders
- Talking to Your Doctor About Medical Cannabis
- Complementary Treatments Worth Discussing With Your Doctor
Diseases in the digestive tract are collectively grouped into a broad category called digestive disease. Health complications may vary from mild to severe, with some of the most common cases being cancer, hernias, gallstones, GI infections, lactose intolerance, diverticular disease, IBD and IBS, heartburn and peptic ulcer disease, cholecystitis, and cholangitis, among many others.
Data from the NIDDK suggests that 60 to 70 million people are affected by all digestive diseases (9). The digestive system plays an important role in overall health. It breaks down and absorbs nutrients from food and drink, including carbohydrates, fats, proteins, minerals, and various vitamins. It also balances healthy microbes and bacteria that are important for mental health, inflammation, and weight management.
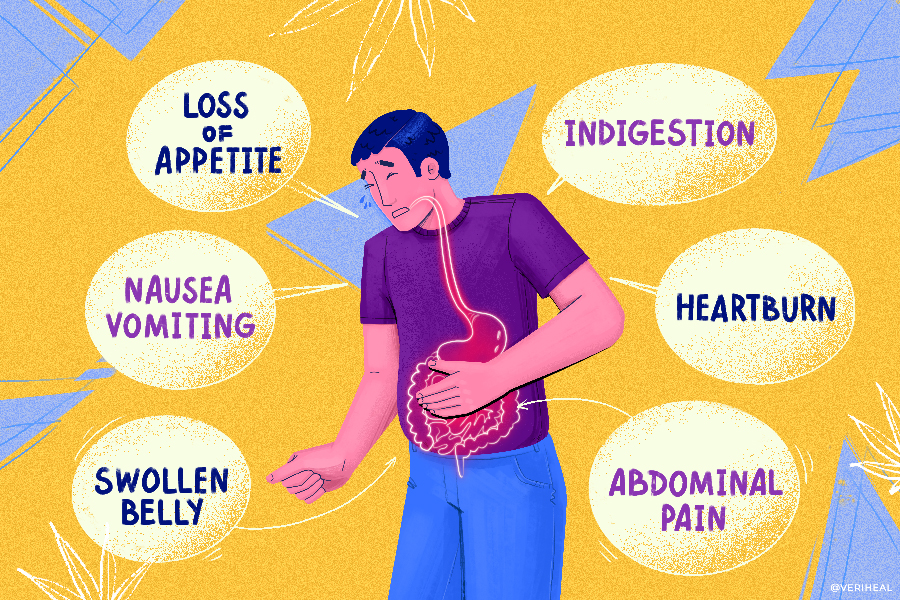
Without maintaining proper digestive health, you may be susceptible to a wide range of unpleasant symptoms, including abdominal pain, bloating, constipation, and indigestion. If symptoms linger for longer than two days, it should be taken as a warning of more serious underlying health problems, such as inflammatory bowel disease or an infection.
When investigated in a lab, cannabis-derived compounds called cannabinoids, including cannabidiol (CBD) and delta-9 tetrahydrocannabinol (THC), appear to possess some anti-inflammatory effects.
Since the digestive tract contains numerous molecules that bind with THC, CBD, enzymes, inflammatory cells, movement receptors, and other natural substances, it’s clear that medical marijuana use affects the digestive tract. When used alongside prescribed medicine, the recovery process for digestive disorders could be more manageable.
Digestive Disorders: Signs, Symptoms and Types
Talking about digestive disorders is not something that most people want to do. However, if you take the appropriate steps to discuss the symptoms of this potential medical condition with a doctor, you can benefit from appropriate diagnosing, treatment, symptomatic relief, and improved quality of life.
Making yourself aware of the most prevalent symptoms of digestive conditions will help you pinpoint a problem before it becomes severe.
If you believe that you may have one of the following health issues, or any other health concerns, consult with a licensed healthcare professional for further assistance:
- Celiac disease
- Crohn disease
- Diverticulitis
- Gastroesophageal reflux disease (GERD)
- Hiatal hernia
- Intestinal problems, such as polyps and cancer
- Infections
- Intestinal ischemia
- Malabsorption
- Peptic ulcer disease
- Short bowel syndrome
- Ulcerative colitis
- Severe nausea, vomiting, diarrhea, or pain that doesn’t go away
Digestive Disorders: Causes and Complications
The triggers that spark the onset of a digestive disorder depend on each individual case. When a patient contracts a virus or bacteria makes its way into the digestive tract, an infection could arise. Inflammation, poor circulation, and lactase deficiency are some other possible causes.
Consuming anti-inflammatory drugs could increase the chances of having a digestive problem and if you’ve already been diagnosed with gallstones, kidney, liver, or muscle dysfunction, the risk is higher. Typical anti-inflammatory drugs are usually not meant to be taken for a long time.
Structural abnormalities in the digestive system and genetics may also influence the risk factor for digestive disorders. Stress has also been shown to cause digestive complications with one medical review, “Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options,” revealing that stress may cause alterations in gastrointestinal motility and increase visceral perception, or noticable pain (5).
If you notice one of the following signs and symptoms of digestive disorders, arrange a consultation with your doctor for a medical examination:
- Bleeding
- Belly pain
- Bloating
- Constipation
- Diarrhea
- Heartburn
- Incontinence/bladder problems
- Nausea/vomiting
- Abnormal, black, or tarry stools
While some digestive disorders fall into the ‘serious’ category and may have long-lasting implications on overall health, others may disappear without treatment. In serious cases, however, it is unlikely that the symptoms of digestive disorders will resolve on their own.
Such complications include — but are not limited to — gastrointestinal bleeding, bowel perforation or infarction, cholecystitis, and inflammation. A poorly functioning digestive system can also contribute to less appetite, weight loss, and problems with maintaining blood sugar levels and nutrition among many other consequences.
According to the findings of a study published in Effects of Digestive Disorders by Somnath Pal, BS (Pharm), MBA, PhD Professor of Pharmacy Administration College of Pharmacy & Health Sciences, St. John’s University in 2013, GI infections were the most frequently reported type of digestive disease (135 million patients or 33% of all patients with digestive disorders) (8).
Of the 67% that were leftover from the initial findings, 87 million patients had hemorrhoids, 63 million had chronic constipation, 62 million had GERD, 20 million had gallstones, 15.3 million had IBS, and 15.5 million were battling the symptoms of peptic ulcer disease (PUD). Overall, GI disorders represent a significant and common health burden.
Digestive Disorders Treatment: Can Cannabinoids Provide Relief?
Cannabis is a genus of plant that grows in three varieties: Cannabis indica, Cannabis sativa, and Cannabis ruderalis. The potent trichome — and cannabinoid-laden flowering herb boasts a long history of medicinal use, not to mention recreational, industrial, and nutritional use across the globe.
One of the most therapeutically-rich varieties of cannabis is the subspecies sativa, which naturally produces aromatic hydrocarbon compounds called cannabinoids. The gastrointestinal tract (GI) is home to 70% of the immune system and studies have proven that the digestive system contains high amounts of endocannabinoids.
Embedded within the GI tract are cannabinoid receptors. Preliminary studies into cannabinoids like Cannabigerol (CBG) and Cannabichromene (CBC) suggest that gut health could be enhanced with frequent cannabinoid administration (10).
Plus, since THC, CBN, CBG, and CBCA can stimulate hunger levels, patients with IBD may regain their appetites using cannabis. Although the vast majority of research into cannabis’ effect on the GI involves IBD, the findings could be of great help to people who suffer from other types of digestive disorders.
In research surveys, many IBS and IBD patients report that medicinal marijuana can be used with success (7, 2). A review in Cannabis and Cannabinoid Research points out “some investigations have demonstrated that patients perceive that cannabis helps to address several symptoms, including reduced appetite, nausea, diarrhea, abdominal pain, and joint pain.”
Studies on the endocannabinoid system, which regulates numerous key bodily and has been shown to play a crucial role in the pathogenesis of IBD, demonstrated a therapeutic effect when tested on mouse colitis rodent subjects (1).
Unfortunately, such a direct impact on gut pathophysiology has not yet been seen in the human gut. The same study in Cannabis and Cannabinoid Research states “To date, no human study has demonstrated that cannabis has a definitive impact on gastrointestinal inflammation in IBD (2).” However, the study also notes there appears to be an inverse association between cannabis use and IBD-related complications.
Nevertheless, patients continue to self-report relief, supported by other underlying scientific evidence. A report titled “Role of Cannabis in Digestive Disorders” found that the role of cannabis in the gut, liver, and pancreas is quite significant. The plant’s effects also indicate its ability to tackle other GI symptoms, including anorexia, chronic abdominal pain, nausea, vomiting, and weight loss (3).
While the literature adds strength to this area of medicinal cannabis research, the report emphasizes the fact that the clinical efficacy of using cannabis and its active components for the treatment of GI disorders remains uncertain.
The Role of the Endocannabinoid System in Treating Digestive Disorders
All living mammals — and animals with a vertebrae — are equipped with an endocannabinoid system (ECS). Scientists only dug up evidence of the ECS’s existence when they first identified the CB1 receptor in 1988. As a fairly new discovery, further research is needed to properly highlight its connection to the digestive system (4).
This network of receptors, endogenous cannabinoids (endocannabinoids), and the enzymes responsible for endocannabinoid synthesis and degradation has a job to make and use cannabinoids that help the body’s basic functions to steadily reach their maximum potential, such as gut health, memory processes, sleep, mood, and appetite.
When a cannabinoid is attached to a CB1 or CB2 receptor, the ECS’s therapeutic benefits can be felt. The receptors bind to body-produced cannabinoids (endocannabinoids) and plant-produced cannabinoids (phytocannabinoids). Phytocannabinoids can also attach to cholinergic and TRPV1 receptors that help manage gut movement, secretions, and pain perception (7).
A vast spectrum of data shows that the complex system carries out the following roles in the GI tract:
- Pain
- Stomach acid regulation
- Satiety (feeling full after eating)
- Motility (ability to transfer food from the mouth and out of the body as a bowel movement)
- Visceral sensation (ability to distinguish bodily organs)
- Inflammation (immune response)
- Pain
Furthermore, a 2008 review showed that there is a lack of CB2 receptors in the inner lining of healthy digestive systems. Inflammation and bowel disease causes the CB2 receptor — which is most common on immune cells — levels to rise. This is a sign that cannabinoid therapy could be useful in cases of inflammatory gastrointestinal disease. (12)
In addition to the regulatory role of the ECS in the gut, the digestive tract may also play an important role in the gut-brain-microbiota axis influencing mood, mental and overall health. Gut dysregulation can bring about chronic inflammation and neuroinflammation. Research into cannabis and gut-brain axis suggests that “Cannabis along with the naturally occurring endocannabinoids has antioxidant and anti-inflammatory properties that can support healing and restoration as an adjunctive therapy (11).”
What Preparations of Cannabis are Best for Digestive Disorders?
If you are seeking relief from the symptoms of digestive disorders and are contemplating the use of cannabis, you’ll need to find a type of cannabis preparation that suits you.
Listed below are some popular types of cannabis preparations and their benefits:
- Edibles
- Pills, capsules, and tablets
- Powder Cannabis
- Vapes
- Tinctures
- Suppositories
Targeting the gut may reasonably be done with tinctures and edible routes that can help coat the inner lining. Suppositories are another route that can help deliver localized relief to the GI tract with a higher bioavailability. Many older patients and those with cachexia, swallowing, extreme nausea, or feeding difficulties can find suppositories to be advantageous without compromising the respiratory system. Suppositories may be difficult to procure and expensive, but can also be made at home with simple ingredients.
Talking to Your Doctor About Medical Cannabis
Finding a solution to your digestive problems requires a diagnosis and medical examination. A healthcare practitioner, specialist, or primary care doctor may carry out an examination to get to the depths of the disorder and find a recommended treatment based on the symptoms.
Once a diagnosis has been made by your doctor, you can kick-off the discussion about the medical uses of cannabis for digestive disorders. However, you should never replace other types of doctor-prescribed medications with medical marijuana.
Instead, cannabis should be implemented into your health and wellness routine as a complementary treatment.
Complementary Treatments Worth Discussing with Your Doctor
Complementary medicine is a term used to describe treatments that can be used alongside traditional Western medicine. The National Center for Complementary and Integrative Health is one example of a government agency that investigates new methods of complementary and alternative medicine.
Diet and lifestyle changes should be considered a priority when you’re searching for complementary medicines to relieve digestive disorders. For example, reducing your intake of fatty foods, quitting smoking, eating and drinking more slowly, engaging in regular exercise, reducing stress, and avoiding chewing gum sweeteners, and foods that cause gas are some approaches that you can try in conjunction with conventional medicines.
Other types of complementary medicine include massage, meditation, biofeedback, tai chi, reiki, music therapy, guided imagery and dietary supplements. Plus, according to Gastroenterology & Hepatology, ginger, peppermint, and probiotics work well as complementary medicines in cases of irritable bowel syndrome (IBS) (6).
You might also consider trying medical cannabis, which could relieve pain and inflammation caused by digestive disorders. Although they can prove beneficial, it’s important that you continue using any medication(s) that are prescribed by your doctor.
Note: The content on this page is for informational purposes only and is not intended to be professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided. Always consult a physician before making any decision on the treatment of a medical condition.
1. Ahmed, W., & Katz, S. (2016). Therapeutic Use of Cannabis in Inflammatory Bowel Disease. Gastroenterology & hepatology, 12(11), 668–679. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5193087/
2. Coates, M. D., Dalessio, S., Walter, V., Stuart, A., Bernasko, N., Tinsley, A., Razeghi, S., Williams, E. D., Clarke, K., & Vrana, K. (2022). Symptoms and extraintestinal manifestations in active cannabis users with inflammatory bowel disease. Cannabis and Cannabinoid Research, 7(4), 445–450. https://www.liebertpub.com/doi/10.1089/can.2020.0155
3. Goyal, H., Singla, U., Gupta, U., & May, E. (2017). Role of cannabis in digestive disorders. European Journal of Gastroenterology & Hepatology, 29(2), 135–143. https://pubmed.ncbi.nlm.nih.gov/27792038/
4. Howlett, A. C., & Abood, M. E. (2017). CB 1 and CB 2 receptor pharmacology. Cannabinoid Pharmacology, 169–206. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5812699/
5. Konturek, P. C., Brzozowski, T., & Konturek, S. J. (2011). Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 62(6), 591–599. https://pubmed.ncbi.nlm.nih.gov/22314561/
6. Nguyen, L., & Director, C. A. P. C. (n.d.). Complementary and alternative medicine for the management of Irritable Bowel Syndrome. Gastroenterology Hepatology. Retrieved September 27, 2022, from https://www.gastroenterologyandhepatology.net/archives/september-2018/complementary-and-alternative-medicine-for-the-management-of-irritable-bowel-syndrome/#:~:text=Ginger%2C%20peppermint%2C%20and%20probiotics%20or,among%20other%20guided%2Dimagery%20exercises.
7. Russo, E. B. (2016). Clinical endocannabinoid deficiency reconsidered: Current research supports the theory in migraine, fibromyalgia, irritable bowel, and other treatment-resistant syndromes. Cannabis and Cannabinoid Research, 1(1), 154–165. https://www.liebertpub.com/doi/10.1089/can.2016.0009
8. Somnath Pal, B. S. (P. (2013, December 18). Effects of digestive disorders. U.S. Pharmacist – The Leading Journal in Pharmacy. Retrieved September 27, 2022, from https://www.uspharmacist.com/article/effects-of-digestive-disorders
9. U.S. Department of Health and Human Services. (n.d.). Digestive diseases statistics for the United States. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved September 27, 2022, from https://www.niddk.nih.gov/health-information/health-statistics/digestive-diseases
10. Walsh, K. B., McKinney, A. E., & Holmes, A. E. (2021). Minor cannabinoids: Biosynthesis, molecular pharmacology and potential therapeutic uses. Frontiers in Pharmacology, 12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8669157/
11. Wilson, N. L., Peterson, S. N., & Ellis, R. J. (2021). Cannabis and the gut–brain axis communication in HIV infection. Cannabis and Cannabinoid Research, 6(2), 92–104. https://www.liebertpub.com/doi/10.1089/can.2020.0037
12. Wright, K. L., Duncan, M., & Sharkey, K. A. (2008). Cannabinoid CB2 receptors in the gastrointestinal tract: A regulatory system in states of inflammation. British Journal of Pharmacology, 153(2), 263–270. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2219529/