Mitochondrial Disease and Medical Cannabis
- What are the Signs, Symptoms, and Types of Mitochondrial Disease?
- Are Cannabinoids a Good Treatment Option for Mitochondrial Disease?
- What Cannabis Preparations are Best for Mitochondrial Disease?
- Talk to Your Doctor About Mitochondrial Disease Treatments
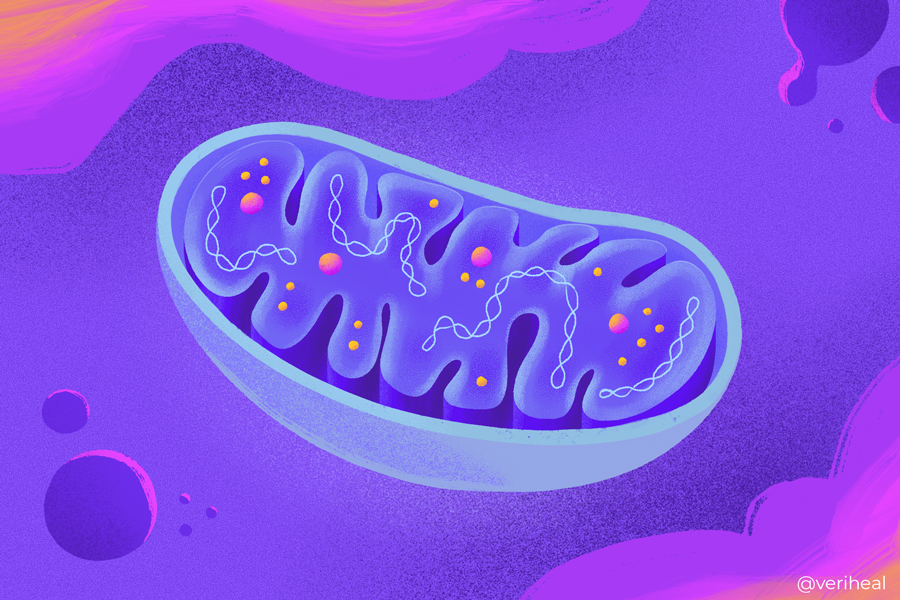
Mitochondrial disease, or mitochondrial disorder (MD), describes a group of disorders affecting the mitochondria. Mitochondria are membrane-bound cell organelles responsible for producing adenosine triphosphate (ATP) — the cell’s energy source (1). Contained in the cytoplasm of all eukaryotic cells, this double-membraned, rod-shaped structure is present in both plant and animal cells.
The main job of mitochondria is to create 90% of the energy required to sustain life and support organ function (17). Every living human has mitochondria, which are found in as many as 1,000 per cell. The mitochondria produce energy through oxidative phosphorylation ranging from 0.5 to 1.0 micrometers in diameter. When mitochondria cannot convert food and oxygen into life-sustaining energy, cell injury, multi-organ failure, and cell death may occur.
Mainly affecting children, MD is one of the most common groups of genetic neuromuscular diseases with a minimum prevalence of greater than 1 in 5,000 adults (11). The disease arises when mitochondrial DNA or nuclear genes become mutated and directly or indirectly disrupt the mitochondrial respiratory chain function.
Supplements like coenzyme Q10, lipoic acid, riboflavin (B12), thiamine (B1), vitamin C, and vitamin E may help treat certain aspects of the disease to an extent. However, there is no definitive cure for mitochondrial disease (6).
Fortunately, thanks to the antioxidant properties of some cannabis compounds (cannabinoids), medical cannabis drugs may offer the potential for symptomatic relief.
What are the Signs, Symptoms, and Types of Mitochondrial Disease?
Mitochondria are the body’s “energy powerhouse”. These cell organelles play an essential role in regulating various biological processes, including cell differentiation, programmed cell death, inflammation, and neurotransmission. There are several diseases associated with mitochondria degradation.
The symptoms of mitochondrial disease depend on which cells are affected. Some of the most common symptoms include:
- Autistic features
- Cramping
- Constipation
- Dementia
- Diabetes
- Diarrhea
- Exercise intolerance
- Gastrointestinal disorders
- Heart, liver, or kidney problems
- Increased risk of infection
- Movement disorders
- Neurological problems (e.g., migraines, seizures, and stroke)
- Lactic acidosis (lactate accumulation from muscles)
- Learning disabilities/developmental delays
- Muscle weakness/pain/low muscle tone
- Poor growth
- Respiratory problems
- Reflux
- Swallowing difficulties
- Thyroid problems
- Vision and/or hearing problems
Examples of primary mitochondrial disease include Autosomal Dominant Optic Atrophy, Alpers Disease or Syndrome, Barth Syndrome, Beta-Oxidation Defects, Carnitine-Acyl-Carnitine Deficiency, Carnitine Deficiency, Coenzyme Q10 Deficiency, Creatine Deficiency Syndromes, Lactic Acidosis
LBSL – Leukodystrophy, LCA Deficiency, LCHA Deficiency, Leigh syndrome, Luft Disease Mitochondrial Deletion Diseases, and Pyruvate Carboxylase Deficiency (16).
Common diseases like Alzheimer’s disease, cancer, diabetes, Lou Gehrig’s disease, and muscular dystrophy have secondary impacts on mitochondria and affect their function as well (9). Since these are not primary mitochondrial diseases, patients don’t need to worry about a worsening course of mitochondrial disease on top of these.
It’s important to note that the severity of MD is based on which area of cells are damaged. Furthermore, symptoms can occur at any age, affect one or more organs, range from mild to severe, and differ among family members.
What Causes Mitochondrial Disease?
Primary mitochondrial disease is a genetic condition that may be inherited in several ways. To paint a clearer picture of inheritance types, it’s wise to learn about genes and DNA. Genes are the basic units of inheritance. These substances contain DNA, which could be described as the “blueprint” that makes each person look unique, such as with their specific eye and hair color.
Understanding how mitochondrial disease is inherited makes it easier to determine the chance of it being passed on to future offspring. In normal circumstances, children inherit genes in pairs, with one from the mother and one from the father. A child who suffers from mitochondrial disease does not receive a normal pair of genes from the parents. Instead, the gene becomes mutated.
Inheritance may occur due to random mutations or the following:
- Autosomal recessive inheritance: One mutated copy of the gene is passed on to a child from both parents. The chances of each child in the family developing mitochondrial disease via autosomal recessive inheritance rest at around 25%.
- Autosomal dominant inheritance: One mutated copy of the gene is passed on to a child from either parent. The chances of each child in the family developing mitochondrial disease via autosomal recessive inheritance rest at around 50%.
- Mitochondrial inheritance: In addition to our cells having DNA, mitochondria also have their own unique form of DNA. Conditions caused by a mutation in the mitochondrial DNA are inherited only from the mother and have a 100% chance of being passed on. The condition is transmitted through the biological female to their children. If a biological male has a mutation in the mitochondrial DNA and the biological female partner doesn’t, their offspring will not inherit the trait.
- Random Mutations: Simply by chance, nuclear or mitochondrial DNA can mutate independently and is not inherited from either parent (9).
Are Cannabinoids a Good Treatment Option for Mitochondrial Disease?
Georgia became the first U.S. state to permit the use of cannabis oil for mitochondrial function. Medical marijuana may help patients with mitochondrial disease to maintain the balance of autophagy and apoptosis in cells in myriad ways. Certain cannabinoids have been shown to affect mitochondrial function due to their antioxidant effects (8).
According to Dr. Fran Kendal — a Harvard-trained board-certified Clinical Biochemical Geneticist who founded the first clinical mitochondrial disease program in the U.S. — the most abundantly therapeutic cannabinoids in mitochondrial disease patients are CBD, THC, and THCa. These cannabinoids may offer symptomatic relief for many co-occurring problematic issues with muscle spasms, pain, appetite, nausea and vomiting, neuroprotection, inflammation, oxidation, and seizures (3).
Scientific data claims that CBD and THC may affect mitochondria and influence cellular function (7). The apparent mitochondrial site of action of CBD has led researchers to believe that CBD may exert neuroprotective properties against cellular and mitochondrially-acting toxins. CBD regulates calcium homeostasis and mediates neuroprotection in neuronal preparations (13).
Small doses of the psychoactive compound THC can amplify mitochondrial activity by interacting with the mitochondrial membrane and promoting ATP creation. This process also promotes cell regeneration by encouraging the process of autophagy that repairs damaged cell parts.
When consumed in higher doses, THC can reduce mitochondrial activity and decrease oxidative stress by binding to CB1 receptors. However, a 2015 study for BioMed Research International indicates that THC may negatively affect mitochondria in the brain (18).
Separate research from GreenBridge Medical suggests that THC-A helps promote mitochondrial energy formation and could benefit people with mitochondrial disease (15). THC-A is the precursor to THC. The potent PPARγ agonist boasts neuroprotective and anti-inflammatory activity (10).
How Does the Endocannabinoid System (ECS) Play a Role in Treating Mitochondrial Disease?
The endocannabinoid system (ECS) is a complex neuromodulatory system that regulates numerous cellular and physiological processes by activating receptors targeted by endocannabinoids or exogenous agonists. Two main receptors are inside the ECS are CB1 and CB2 (4).
During the early 1990s, researchers exploring cannabis’ primary psychoactive cannabinoid THC discovered this complex cell-signaling system. One of the main roles of the ECS is modulating mitochondrial function (4). What’s more, plant-derived cannabinoids may target more receptors than these and also different mitochondrial processes.
A growing body of evidence has highlighted the potential advantages of using cannabinoids to modulate mitochondrial processes, such as activation of the intrinsic apoptotic pathway, disruption of mitochondrial respiration and ATP production,
regulation of intracellular calcium levels and mitochondrial dynamics, as well as deterioration of electron transport chain activity (5).
Certain cannabinoids can activate CB1 receptors localized at the mitochondrial membranes or plasma. When type 1 cannabinoid receptors present at brain mitochondria membranes (mtCB1) are activated, they can directly alter mitochondrial energetic activity. Cannabinoids may also influence various components of the mitochondrial respiratory chain (2).
What Cannabis Preparations Are Best for Mitochondrial Disease?
One of the main appeals associated with medical cannabis use to treat mitochondrial disease is the diversity in terms of product options. Various cannabis preparations are available to patients, including:
- Infused edibles
- Pills, capsules, and tablets
- Dissolvable cannabis powder
- Transdermal Patches
- Vapes
- Smokable and vaporizable dry flower
- Topical lotions (for localized relief from muscle spasms)
- Tinctures
Talk to Your Doctor About Mitochondrial Disease Treatments
MD diagnosis begins with a series of examinations and tests, one of the most important being a muscle biopsy. This procedure involves removing and examining a small sample of muscle tissue. After being treated with a dye that stains the mitochondria, torn muscle cells (fibers) turn a shade of red.
One of the first steps a doctor will take when dealing with cases of mitochondrial disease involves reviewing a patient’s family history. Common diagnostic tests that may be conducted by a doctor include:
- A full physical examination
- A metabolic examination, e.g., blood tests, cerebral spinal fluid tests (spinal tap), and urine tests
- A neurological examination
- Audiogram or auditory-brainstem evoked responses (ABER) for hearing symptoms
- Blood test to spot thyroid dysfunction
- Blood test for genetic DNA testing
- Electrocardiogram (EKG) or echocardiogram to detect symptoms of heart disease
- Magnetic resonance imaging (MRI) or spectroscopy (MRS) to assess neurological symptoms
- Retinal exam or electroretinogram (ERG) to assess visual symptoms.
Complementary Treatments Worth Discussing with Your Doctor
Many experts opt for recommending a combination of antioxidants and vitamins, such as coenzyme Q10, to amplify health and nutrition in patients with mitochondrial disease (12). Foods like broccoli, cauliflower, chicken, oily fish, grass-fed beef, and sesame seeds are rich in CoQ10, which has been shown to facilitate mitochondrial function.
In addition to eating well, patients diagnosed with MD may consider following a carefully prescribed exercise and physical or occupational therapy regimen to promote mitochondrial repair, activities of daily living and functioning, and muscle regeneration. Moreover, a handful of preclinical studies suggest that low-level laser therapy may encourage mitochondrial activity and ATP synthesis, although this is still in the experimental stage (14). The efficacy of using these therapies to change the course of the disease has not yet been proven.
The correct combination of vitamins may help to prevent the symptoms of MD from worsening amid moments of physiologic stress and illness. Medical marijuana also presents promise as a tool for mitigating some of the symptoms of MD. However, it’s important that you continue using any medication(s) and treatments prescribed by your doctor.
Note: The content on this page is for informational purposes only and is not intended to be professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided. Always consult a physician before making any decision on the treatment of a medical condition.
1. Admin. (2022, September 22). What is mitochondria (structure, Diagram & function). BYJUS. Retrieved February 15, 2023, from https://byjus.com/biology/mitochondria/
2. Hebert-Chatelain, E., Desprez, T., Serrat, R., Bellocchio, L., Soria-Gomez, E., Busquets-Garcia, A., Pagano Zottola, A. C., Delamarre, A., Cannich, A., Vincent, P., Varilh, M., Robin, L. M., Terral, G., García-Fernández, M. D., Colavita, M., Mazier, W., Drago, F., Puente, N., Reguero, L., … Marsicano, G. (2016). A cannabinoid link between mitochondria and memory. Nature, 539(7630), 555–559. https://www.nature.com/articles/nature20127
3. Kendall, F. (n.d.). Summary – Medical Cannabis and Mitochondrial Disease. Medical Cannabis and Mitochondrial Disease. Retrieved February 15, 2023, from https://www.mitoaction.org/wp-content/uploads/2019/03/Summary-Medical-Cannabis-and-Mitochondrial-Disease-Kendall.pdf
4. Letscher, E. (2018, November 12). The endocannabinoid system, our universal regulator. Journal of Young Investigators. Retrieved February 15, 2023, from https://www.jyi.org/2018-june/2018/6/1/the-endocannabinoid-system-our-universal-regulator
5. Malheiro, R. F., Carmo, H., Carvalho, F., & Silva, J. P. (2023). Cannabinoid-mediated targeting of mitochondria on the modulation of mitochondrial function and Dynamics. Pharmacological Research, 187, 106603. https://www.sciencedirect.com/science/article/pii/S1043661822005497
6. Mary Kugler, R. N. (2021, October 27). Mitochondrial disease symptoms and treatment. Verywell Health. Retrieved February 15, 2023, from https://www.verywellhealth.com/mitochondrial-disease-2860396#:~:text=There%20is%20no%20cure%20for%20mitochondrial%20disease.%20Certain,disease.%20Avoiding%20stress%20may%20also%20help%20reduce%20symptoms
7. Mitochondria mysteries. Homeostasis, renewal and the endocannabinoid system. (2016, December 7). Retrieved February 15, 2023, from https://www.projectcbd.org/science/mitochondria-mysteries
8. Mitochondrial disease. Mitochondrial Disease – Marijuana Doctors | Online Medical Card Directory. (n.d.). Retrieved February 15, 2023, from https://www.marijuanadoctors.com/conditions/mitochondrial-disease/
9. Mitochondrial diseases: Causes, symptoms, diagnosis & treatment. Cleveland Clinic. (n.d.). Retrieved February 15, 2023, from https://my.clevelandclinic.org/health/diseases/15612-mitochondrial-diseases
10. Nadal, X., del Río, C., Casano, S., Palomares, B., Ferreiro-Vera, C., Navarrete, C., Sánchez-Carnerero, C., Cantarero, I., Bellido, M. L., Meyer, S., Morello, G., Appendino, G., & Muñoz, E. (2017). Tetrahydrocannabinolic acid is a potent PPARΓ agonist with neuroprotective activity. British Journal of Pharmacology, 174(23), 4263–4276. https://pubmed.ncbi.nlm.nih.gov/28853159/
11. Ng, Y. S., & Turnbull, D. M. (2015). Mitochondrial disease: Genetics and management. Journal of Neurology, 263(1), 179–191. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4723631/
12. Parikh, S., Saneto, R., Falk, M. J., Anselm, I., Cohen, B. H., & Haas, R. (2009). A modern approach to the treatment of mitochondrial disease. Current Treatment Options in Neurology, 11(6), 414–430. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3561461/
13. Ryan, D., Drysdale, A. J., Lafourcade, C., Pertwee, R. G., & Platt, B. (2009). Cannabidiol targets mitochondria to regulate intracellular ca2+ levels. Journal of Neuroscience, 29(7), 2053–2063. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6666323/
14. Silveira, P. C. L., Silva, L. A., Fraga, D. B., Freitas, T. P., Streck, E. L., & Pinho, R. (2009). Evaluation of mitochondrial respiratory chain activity in muscle healing by low-level laser therapy. Journal of Photochemistry and Photobiology B: Biology, 95(2), 89–92. https://www.sciencedirect.com/science/article/abs/pii/S1011134409000049
15. THC-A and mitochondria. THC-A AND MITOCHONDRIA: GreenBridge Medical: Family Medicine Physicians. (n.d.). Retrieved February 15, 2023, from https://www.greenbridgemed.com/blog/thc-a-and-mitochondria
16. Types of mitochondrial disease. UMDF. (n.d.). Retrieved February 15, 2023, from https://www.umdf.org/what-is-mitochondrial-disease-2/types-of-mitochondrial-disease/
17. Understanding & navigating mitochondrial disease. UMDF. (n.d.). Retrieved February 15, 2023, from https://www.umdf.org/what-is-mitochondrial-disease-2/
18. Wolff, V., Schlagowski, A.-I., Rouyer, O., Charles, A.-L., Singh, F., Auger, C., Schini-Kerth, V., Marescaux, C., Raul, J.-S., Zoll, J., & Geny, B. (2015). Tetrahydrocannabinol induces brain mitochondrial respiratory chain dysfunction and increases oxidative stress: A potential mechanism involved in cannabis-related stroke. BioMed Research International, 2015, 1–7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4310259/