Medical Cannabis & Sickle Cell Disease: What is the Connection?
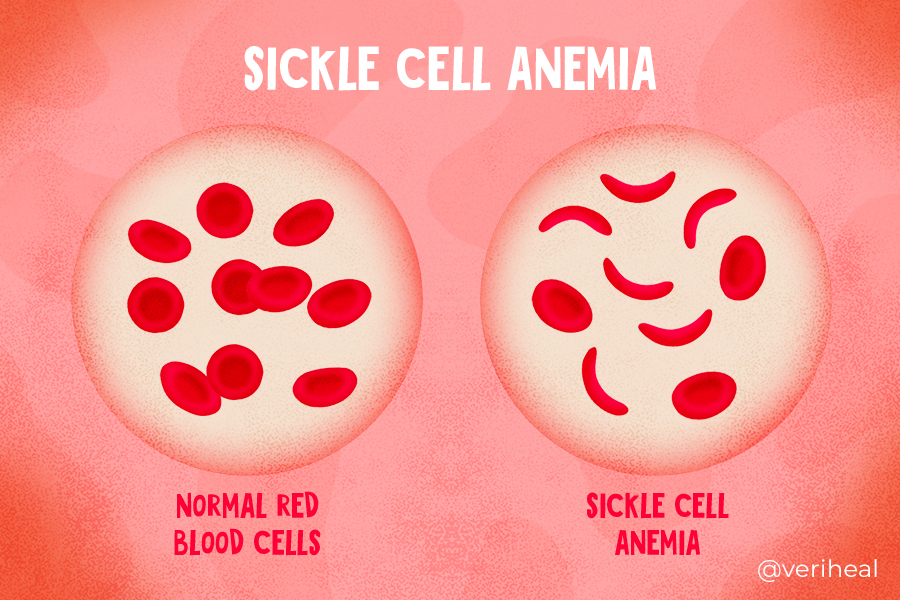
Sickle cell disease (SCD) is a group of inheritable disorders that impact the way that the body produces and uses hemoglobin. It plays a large role in the body’s ability to produce red blood cells and causes them to have a sickle shape. This sickle shape leads to recurring painful episodes requiring hospitalization called “sickle cell crisis”. Sickle cell crisis causes severe pain, inflammation, and an increased risk for severe infections.
Sickle Cell Disease is a qualifying condition for medical marijuana certification in many states. Thankfully medical cannabis can address many of these issues caused by SCD. Clinical trials regarding the use of medical marijuana in this area has been conducted since the 1990s, which provides us with some clues on how patients with SCD may benefit from medical cannabis treatments.
Medical cannabis contains over 120 naturally-occurring and medicinal compounds called cannabinoids. The most well-known cannabinoids are Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD). When cannabinoids are used, they make contact with receptors of the endocannabinoid system. These receptors include CB1 & CB2, transient receptor potential vanilloid (TRPV), peroxisome proliferator-activated receptors (PPARs), and other receptors that make up the endocannabionoidome (eCBome). These receptors are located in a variety of tissues and organs and are responsible for interacting with fatty-based neurotransmitters called endocannabinoids.
Endocannabinoids are responsible for regulating a variety of processes in the body including pain perception, how the body deals with inflammation, and the body’s ability to maintain homeostasis or proper body temperature. Cannabinoids from plants (phytocannabinoids) can work on the same receptors to help bring relief.
- Targeting the ECS for Sickle Cell Disease
- Cannabinoids for Sickle Cell Disease Symptoms
- What Does the Science Say?
- Using Medical Cannabis for Symptoms of Sickle Cell Disease
- What is Sickle Cell Disease?
Targeting The ECS for Sickle Cell Disease
Pain in SCD is complex and occurs via nociceptive, inflammatory, and neuropathic pathways (44). These are all pathways that medical cannabis may be used to relieve pain.
Cannabinoid receptors CB1 &CB2 are present in large quantities throughout the body. These receptors are present on nerve cells as well as on cells that are responsible for causing inflammation (46). When inflammation occurs in the body, the immune system sends out pro-inflammatory, pain-sensitizing signals to recruit cells to heal the affected part of the body.
Unfortunately, when a patient is experiencing chronic pain, pain sensitivity is heightened, and this makes them even more susceptible to pain. Researchers have found that a type of immune cell called a mast cell increases pain sensitivity (47,7). Mast cells are known for releasing neuromodulators, such as histamine that is released during an allergic reaction. When these neuromodulators are released, they excite nerve cells called nociceptive neurons, making them more sensitive to the stimuli of pain.
The problem is that when patients receive morphine and opioids to treat pain, the mast cells are activated, causing heightened pain sensitivity (46). This can create almost a rebound effect for pain.
Researchers have found that slowing down mast cell activation can have analgesic effects in sickle cell disease patients (47, 46). This process has been shown to be effective with medical marijuana use. It is also used in pharmaceutical medications such as cromolyn and imatinib which suppress the immune system (44).
Cannabinoids for Sickle Cell Disease Symptoms
Because of the effects of cannabis on pain and modulating the immune system, SCD patients may experience improvements in the following areas:
- Chronic pain & acute pain
- Neuropathy
- Inflammation
- Infections
- Skin lesions
- Insomnia
- ER visits
- Hospitalizations
- Depression
- Found in around 35% of SCD patients, leading to worsening physical, mental health, and economic outcomes in this group (2).
What Does the Science Say?
Animal studies regarding sickle cell anemia have provided much insight into how pain in SCD can be controlled through the ECS. One such study provided researchers with the basics regarding the role of mast cells in pain. This 2016 study compared mice with HbSS sickle cell disease against mice without (46). These mice were treated with the cannabinoid receptor agonist CP 55,940 which activated both CB1 & CB2 receptors. They were also treated with medications that would activate only one cannabinoid receptor at a time.
During this study, the mice were evaluated for pain-related behaviors and neurogenic inflammation. These mice were exposed to low-oxygen and re-oxygenation cycles. The researchers took blood flow measures, skin biopsies, and had blood tests taken to examine hematocrit, total hemoglobin, complete blood cells count, and red cell indices (a measure of sickle cell percentages) (46).
The researchers found that cannabinoids reduced neurogenic inflammation, slowed down the granulation of mast cells, and mitigated pain in this preclinical study (46). This data has served as an important basis for treating human patients with sickle cell disease.
A 2020 study conducted on humans examined the use of cannabis in patients with sickle cell disease. This was based on self-reported data from patients with HbSS, HbSC, HbS beta⁰, and HbS beta⁺ (19). Researchers were interested in examining the effects and use in participants with severe or acute SCD. They found that daily cannabis users had fewer emergency room visits and fewer hospitalizations than patients who did not use cannabis products frequently or were identified as non-users.
These results are interesting because daily consumers reported higher pain levels than the other groups when compared by age, gender, and type of SCD (19). Researchers believe that people with severe types of SCD were more likely to be daily cannabis consumers and more likely to try cannabis for pain relief. This information has been used as background information for a study examining SCD and inhaled cannabis as well as a study on SCD and dronabinol.
Using Medical Cannabis for Symptoms of Sickle Cell Disease
Since May 2022, there have not been any large-scale studies examining the use of cannabis and its cannabinoids on the SCD population (15). This review published in Cureus found that the studies using medical cannabis over other medications have mixed results. Some studies show the benefits while other studies do not, meaning a definite recommendation about medical cannabis use is unable to be made currently.
Standard treatment for sickle cell disease includes pain medications, stem cell therapy, and blood transfusions. Medical marijuana could be used alongside these treatments for further analgesic results.
More research in this area is needed, as patients with sickle cell disease experience increased health issues and medical risks when compared to the general population. That being said, many states are including SCD as a condition that can be treated with medical cannabis (29). Medical cannabis is seen as a treatment option for patients as an alternative to opioids.
Before using medical marijuana to manage the symptoms of sickle cell disease, have a conversation with your doctor or a trusted healthcare professional about integrating it into your treatment plan. Marijuana use can cause undesirable side effects when used alongside certain medications. As a result, it’s important to be transparent with your physician about the current medications you’re taking, as well as any medical or illicit marijuana use.
What is Sickle Cell Disease?
Sickle cell disease (SCD) is a group of inheritable red blood cell disorders that impact hemoglobin. Hemoglobin is a protein found in red blood cells that is responsible for transporting oxygen as the blood circulates around the body (40). Red blood cells are typically disc-shaped and are flexible in order to move through blood vessels.
In patients with SCD, the red blood cells are not flexible and have a crescent or sickle shape. These cells can block blood flow to other parts of the body, resulting in hypoxia, or low blood oxygen (38). Cells that are affected by sickle cell disease die early, leading to a shortage in the number of red blood cells a patient has (12).
SCD is considered a multisystem disorder and is the most common genetic disease in the United States (38). It is most prevalent in African Americans and people descending from Sub-Saharan Africa, South Asia, the Middle East, and the Mediterranean.
SCD Symptoms
Sickle cell disease is present in patients at birth but does not show symptoms during the first 6 months of life because of the presence of fetal hemoglobin, which then decreases with aging (38). The first signs in pediatric patients include dactylitis, or painful swelling in the hands and feet, extreme tiredness & fussiness, and jaundice (49). For these reasons, newborns in all 50 states and the District of Columbia are screened for sickle cell disease within 24-48 hours after birth as recommended by the CDC.
The exact symptoms of sickle cell disease vary depending on which body systems are affected and can affect quality of life in various ways. Some patients are asymptomatic while other patients experience severe symptoms (38). SCD symptoms include (42):
Systemic Symptoms
- Chronic pain
- Acute pain crisis, also known as vaso-occlusive crisis, which causes sharp, intense pain in different parts of the body due to blocked blood flow
- Delayed growth and puberty onset
- Increased risk for infections if the spleen is damaged
- Pregnancy complications include an increased risk of high blood pressure, blood clots, miscarriage, premature birth, and low infant birth weight
- Avascular or aseptic necrosis, which causes blood loss and pain in the joints such as the hip, shoulders, knees, and ankles
Location Specific Symptoms
- Acute chest syndrome is caused by blocked blood flow to the lungs and leads to chest pain, fever, and breathing difficulties. It is considered a medical emergency
- Enlarged spleen
- Decreased eye functionality including retina detachment and vision loss
- Gallstones
- Heart disease and pulmonary hypertension
- Kidney complications causing increased urine output
- Skin ulcers on the legs
- Sickle cell intrahepatic cholestasis causes severe liver damage when blood flow is blocked in the liver
- Priapism, an unwanted and prolonged painful erection. This is considered a medical emergency if it lasts longer than 4 hours.
- Stroke
Anemia Complications
- Aplastic crisis
- This is caused by an infection of parvovirus B19 and leads to red blood cell production being stopped in the bone marrow of sickle cell disease patients. This causes severe anemia.
- Splenic sequestration crisis
- This occurs when sickle-shaped red blood cells get stuck in the spleen, causing the spleen to enlarge and not enough blood cells to circulate through the rest of the body.
Types of Sickle Cell Disease
There are several different types of sickle cell disease that depend on the specific genetic traits a person inherits (12). Every type of SCD has an impact on how the body produces hemoglobin.
HbSS
This type of SCD occurs when a person inherits two copies of the gene for hemoglobin S (12). This is commonly called sickle cell anemia as it leads to sickle-shaped red blood cells.
HbSC
Patients with this form of SCD inherit one copy of the hemoglobin S gene and a copy of the hemoglobin C gene (12). HbSC is a milder form of sickle cell disease.
HbS Beta Thalassemia
These patients inherit a hemoglobin S gene from one parent and a gene for beta thalassemia from the other parent. There are two forms of HbS beta thalassemia which include HbS beta⁰ and HbS beta⁺ (12). Patients with HbS beta⁰ usually have a severe form of sickle cell disease while patients with HbS beta⁺ have a milder form.
HbSD, HbSE, & HbSO
HbSD, HbSE, and HbSO are considered rare types of SCD. These patients inherit one hemoglobin S gene and another abnormal gene including hemoglobin D, hemoglobin E, or hemoglobin O (12). The severity of SCD varies for this group of patients.
HbAS
These patients have a sickle cell trait but rarely have any symptoms of SCD (12). These patients inherited a hemoglobin S gene and a hemoglobin A gene. Hemoglobin A is considered a healthy and normal hemoglobin gene. These patients can pass either gene on to their children.
Note: Veriheal does not intend to give this as professional medical advice. Do not attempt to self-diagnose, or prescribe treatment based on the information provided on this page. Always consult a physician before making any decision on the treatment of a medical condition.
1. Abrams, D. I., Couey, P., Dixit, N., Sagi, V., Hagar, W., Vichinsky, E., Kelly, M. E., Connett, J. E., & Gupta, K. (2020). Effect of Inhaled Cannabis for Pain in Adults With Sickle Cell Disease: A Randomized Clinical Trial. JAMA Network Open, 3(7), e2010874. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768349
2. Adam, S. S., Flahiff, C. M., Kamble, S., Telen, M. J., Reed, S. D., & De Castro, L. M. (2017). Depression, quality of life, and medical resource utilization in sickle cell disease. Blood Advances, 1(23), 1983–1992. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5728280/
3. Argueta, D. A., Aich, A., Muqolli, F., Cherukury, H., Sagi, V., DiPatrizio, N. V., & Gupta, K. (2020). Considerations for Cannabis Use to Treat Pain in Sickle Cell Disease. Journal of Clinical Medicine, 9(12), 3902. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7761429/
4. Aron, J. A., Healy, E. W., Robinson, J. R. M., & Blinderman, C. D. (2022). Effects of Medical Cannabis Certification on Hospital Use by Individuals with Sickle Cell Disease. Cannabis and Cannabinoid Research. https://www.liebertpub.com/doi/abs/10.1089/can.2022.0136
5. Ballas, S. K. (2017). The Use of Cannabis by Patients with Sickle Cell Disease Increased the Frequency of Hospitalization due to Vaso-Occlusive Crises. Cannabis and Cannabinoid Research, 2(1), 197–201. https://www.liebertpub.com/doi/full/10.1089/can.2017.0011
6. Bhatt, R., Labus, J., Coloigner, J., Ashe-McNalley, C., Coates, T., Zeltzer, L., & Wood, J. (2018). Patients with sickle cell disease exhibit increased functional connectivity and centrality of the locus coeruleus compared to anemic controls. The Journal of Pain, 19(3), S2–S3. https://www.jpain.org/article/S1526-5900(17)30833-7/fulltext
7. Brandow, A. M., Carroll, C. P., Creary, S., Edwards-Elliott, R., Glassberg, J., Hurley, R. W., Kutlar, A., Seisa, M., Stinson, J., Strouse, J. J., Yusuf, F., Zempsky, W., & Lang, E. (2020). American Society of Hematology 2020 guidelines for sickle cell disease: Management of acute and chronic pain. Blood Advances, 4(12), 2656–2701. https://www.sciencedirect.com/science/article/pii/S2473952920312465
8. Brandow, A. M., Zappia, K. J., & Stucky, C. L. (2017). Sickle cell disease: A natural model of acute and chronic pain. Pain, 158(Suppl 1), S79–S84. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5350013/
9. Cannabinoids for the Reduction of Pain and Inflammation in Sickle Cell Disease—ProQuest. (n.d.). Retrieved March 30, 2023, from https://www.proquest.com/openview/92816e13be658ea54de875570758581c/1?pq-origsite=gscholar&cbl=18750&diss=y
10. Cannabis shows potential for mitigating sickle cell disease pain. (n.d.). ScienceDaily. Retrieved March 30, 2023, from https://www.sciencedaily.com/releases/2020/07/200717133236.htm
11. Cannabis shows potential for mitigating sickle cell disease pain. (2020, July 17). UCI News. https://news.uci.edu/2020/07/17/cannabis-shows-potential-for-mitigating-sickle-cell-disease-pain/
12. CDC. (2022, August 18). What is Sickle Cell Disease? | CDC. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/sicklecell/facts.html
13. Cherukury, H. M., Argueta, D. A., Garcia, N., Fouda, R., Kiven, S., Lei, J., Sagi, V., Velasco, G. J., Avalos, B., DiPatrizio, N. V., & Gupta, K. (2023). Cannabidiol attenuates hyperalgesia in a mouse model of sickle cell disease. Blood, 141(2), 203–208. https://ashpublications.org/blood/article-abstract/141/2/203/486663/Cannabidiol-attenuates-hyperalgesia-in-a-mouse?
14. Conran, N., Saad, S. T. O., Costa, F. F., & Ikuta, T. (2007). Leukocyte numbers correlate with plasma levels of granulocyte-macrophage colony-stimulating factor in sickle cell disease. Annals of Hematology, 86(4), 255–261. https://pubmed.ncbi.nlm.nih.gov/17205286/
15. Cureus | The Efficacy of Marijuana Use for Pain Relief in Adults With Sickle Cell Disease: A Systematic Review | Article. (n.d.). Retrieved March 30, 2023, from https://www.cureus.com/articles/79800-the-efficacy-of-marijuana-use-for-pain-relief-in-adults-with-sickle-cell-disease-a-systematic-review#!/
16. Curtis, S. A., Lew, D., Spodick, J., Hendrickson, J. E., Minniti, C. P., & Roberts, J. D. (2020). Medical marijuana certification for patients with sickle cell disease: A report of a single center experience. Blood Advances, 4(16), 3814–3821. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7448584/
17. Curtis, S. A., Lew, D., Spodick, J., & Roberts, J. D. (2018). Medical Marijuana for Sickle Cell Disease: Results of Two Years of Certification in an Adult Sickle Cell Center. Blood, 132, 858. https://www.sciencedirect.com/science/article/pii/S0006497119369071
18. Curtis, S. A., & Novelli, E. M. (2023). Is CBD ready for prime time in sickle cell disease? Blood, 141(2), 132–133. https://ashpublications.org/blood/article/141/2/132/494014/Is-CBD-ready-for-prime-time-in-sickle-cell-disease
19. Daily Cannabis Users with Sickle Cell Disease Show Fewer Admissions than Others with Similar Pain Complaints | Cannabis and Cannabinoid Research. (n.d.). Retrieved March 30, 2023, from https://www.liebertpub.com/doi/10.1089/can.2019.0036
20. Du, S., Lin, C., & Tao, Y.-X. (2019). Updated mechanisms underlying sickle cell disease-associated pain. Neuroscience Letters, 712, 134471. https://www.sciencedirect.com/science/article/pii/S0304394019305749
21. Early insights into the neurobiology of pain in sickle cell disease: A systematic review of the literature—Brandow—2015—Pediatric Blood & Cancer—Wiley Online Library. (n.d.). Retrieved March 30, 2023, from https://onlinelibrary.wiley.com/doi/abs/10.1002/pbc.25574
22. Effect of Inhaled Cannabis for Pain in Adults With Sickle Cell Disease: A Randomized Clinical Trial | Hematology | JAMA Network Open | JAMA Network. (n.d.). Retrieved March 30, 2023, from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768349
23. Fazzari, F. G. T., & Maida, V. (2021). Comment on “Cannabinoids in dermatologic surgery.” Journal of the American Academy of Dermatology, 85(6), e409–e410. https://www.jaad.org/article/S0190-9622(21)02341-0/fulltext
24. Howard, J., Anie, K. A., Holdcroft, A., Korn, S., & Davies, S. C. (2005). Cannabis use in sickle cell disease: A questionnaire study. British Journal of Haematology, 131(1), 123–128. https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/j.1365-2141.2005.05723.x
25. In Sickle Cell Disease Patients, Marijuana Use Common, Survey Reports. (n.d.). Retrieved March 30, 2023, from https://sicklecellanemianews.com/news/marijuana-use-common-sickle-cell-disease-patients-survey/
26. Kohli, D. R., Li, Y., Khasabov, S. G., Gupta, P., Kehl, L. J., Ericson, M. E., Nguyen, J., Gupta, V., Hebbel, R. P., Simone, D. A., & Gupta, K. (2010). Pain-related behaviors and neurochemical alterations in mice expressing sickle hemoglobin: Modulation by cannabinoids. Blood, 116(3), 456–465. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2913454/
27. Mechanisms of pain in sickle cell disease—Kensuke Takaoka, Asha Caroline Cyril, Sandhya Jinesh, Rajan Radhakrishnan, 2021. (n.d.). Retrieved March 30, 2023, from https://journals.sagepub.com/doi/abs/10.1177/2049463720920682?journalCode=bjpb
28. Medical Marijuana Reduces Hospital Visits Among Sickle Cell Disease Patients. (2020, August 13). HCP Live. https://www.hcplive.com/view/medical-marijuana-reduces-hospital-visits-sickle-cell-disease
29. Minnesota’s medical cannabis program adds sickle cell disease, chronic vocal or motor tic disorder to list of qualifying medical conditions—MN Dept. Of Health. (n.d.). Retrieved April 1, 2023, from https://www.health.state.mn.us/news/pressrel/2020/cannabis120120.html
30. Orhurhu, M. S., Chu, R., Claus, L., Roberts, J., Salisu, B., Urits, I., Orhurhu, E., Viswanath, O., Kaye, A. D., Kaye, A. J., & Orhurhu, V. (2020). Neuropathic Pain and Sickle Cell Disease: A Review of Pharmacologic Management. Current Pain and Headache Reports, 24(9), 52. https://doi.org/10.1007/s11916-020-00885-5
31. PhD, Ö. Ö., MSc. (2022, August 30). New Study to Test Safety and Efficacy of a Cannabinoid in Sickle Cell Disease. Rare Disease Advisor. https://www.rarediseaseadvisor.com/news/scd-news-briefs/study-testing-safety-efficacy-cannabinoid-sickle-cell-disease/
32. Pini, A., Mannaioni, G., Pellegrini-Giampietro, D., Passani, M. B., Mastroianni, R., Bani, D., & Masini, E. (2012). The role of cannabinoids in inflammatory modulation of allergic respiratory disorders, inflammatory pain and ischemic stroke. Current Drug Targets, 13(7), 984–993. https://doi.org/10.2174/138945012800675786
33. Price, S. (2020, August 18). Clinical trial shows potential of cannabis to lessen sickle cell disease pain. Health Europa. https://www.healtheuropa.com/clinical-trial-shows-potential-of-cannabis-to-lessen-sickle-cell-disease-pain/102214/
34. Roberts, J. D., Spodick, J., Cole, J., Bozzo, J., Curtis, S., & Forray, A. (2018). Marijuana Use in Adults Living with Sickle Cell Disease. Cannabis and Cannabinoid Research, 3(1), 162–165. https://www.liebertpub.com/doi/10.1089/can.2018.0001
35. Roy, A. M., Konda, M., Goel, A., & Sasapu, A. (2019). Characteristics of Marijuana Usage in Sickle Cell Patients: A Nationwide Analysis. Blood, 134, 4848. https://www.sciencedirect.com/science/article/pii/S0006497118627740
36. Sagi, V., Lei, J., Kiven, S. B., Tran, H., & Gupta, K. (2019). Cannabidiol Reduces Acute and Chronic Hyperalgesia in Humanized Sickle Mice. Blood, 134, 77. https://www.sciencedirect.com/science/article/pii/S0006497118579957
37. Sagi, V., Mittal, A., Tran, H., & Gupta, K. (2021). Pain in sickle cell disease: Current and potential translational therapies. Translational Research, 234, 141–158. https://www.sciencedirect.com/science/article/pii/S1931524421000578
38. Sedrak, A., & Kondamudi, N. P. (2023). Sickle Cell Disease. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK482384/
39. Sharma, D., & Brandow, A. M. (2020). Neuropathic pain in individuals with sickle cell disease. Neuroscience Letters, 714, 134445. https://www.sciencedirect.com/science/article/pii/S0304394019305488
40. Sickle Cell Disease – What Is Sickle Cell Disease? | NHLBI, NIH. (2022, July 22). https://www.nhlbi.nih.gov/health/sickle-cell-disease
41. Sickle cell disease: MedlinePlus Genetics. (n.d.). Retrieved March 30, 2023, from https://medlineplus.gov/genetics/condition/sickle-cell-disease/
42. Sickle Cell Disease—How Sickle Cell Disease May Affect Your Health | NHLBI, NIH. (2022, July 15). https://www.nhlbi.nih.gov/health/sickle-cell-disease/health-effects
43. Small-Howard, A. L., Shimoda, L. M. N., Adra, C. N., & Turner, H. (2005). Anti-inflammatory potential of CB1-mediated cAMP elevation in mast cells. Biochemical Journal, 388(Pt 2), 465–473. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1138953/
44. Tran, H., Gupta, M., & Gupta, K. (2017). Targeting novel mechanisms of pain in sickle cell disease. Blood, 130(22), 2377–2385. https://ashpublications.org/blood/article/130/22/2377/36562/Targeting-novel-mechanisms-of-pain-in-sickle-cell
45. Uhelski, M. L., Gupta, K., & Simone, D. A. (2017). Sensitization of C-fiber nociceptors in mice with sickle cell disease is decreased by local inhibition of anandamide hydrolysis. Pain, 158(9), 1711–1722. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5561456/
46. Vincent, L., Vang, D., Nguyen, J., Benson, B., Lei, J., & Gupta, K. (2016). Cannabinoid receptor-specific mechanisms to alleviate pain in sickle cell anemia via inhibition of mast cell activation and neurogenic inflammation. Haematologica, 101(5), 566–577. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5004356/
47. Vincent, L., Vang, D., Nguyen, J., Gupta, M., Luk, K., Ericson, M. E., Simone, D. A., & Gupta, K. (2013). Mast cell activation contributes to sickle cell pathobiology and pain in mice. Blood, 122(11), 1853–1862. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3772495/
48. Zheng, C. Y., Minniti, C. P., & Chaitowitz, M. H. (2016). Sickle Cell Crisis Complicated by Synthetic Cannabinoid Abuse: A Case Report. Hemoglobin, 40(3), 220–222. https://www.tandfonline.com/doi/full/10.3109/03630269.2016.1149077
49. Sickle Cell Disease—Symptoms | NHLBI, NIH. (2022, July 14).https://www.nhlbi.nih.gov/health/sickle-cell-disease/symptoms